Child and Adolescent Psychiatry
(038) A Curious Incident of TikTok "Psychosis" in a Patient with Intellectual Disability
- MF
Matthew Fiorillo, DO (he/him/his)
Child Psychiatry Fellow
Ann & Robert H. Lurie Children's Hospital of Chicago
Chicago, Illinois .jpg)
Ewa D. Bieber, MD (she/her/hers)
Child and Adolescent Psychiatrist
Ann & Robert H. Lurie Children's Hospital of Chicago
Chicago, Illinois
Presenting Author(s)
Co-Author(s)
Background/Significance: Intellectual Disability (ID) is a condition characterized by impaired intellectual and adaptive functioning. The prevalence of co-occurring mental health disorders, including psychotic disorders, in ID is higher than in the general population. Optimal evaluation and treatment of psychiatric illness in ID requires the clinician to collect a detailed developmental history.
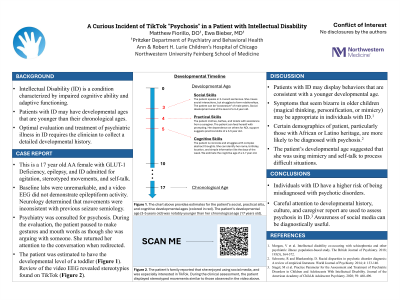
Case: A 16-year-old African-American woman with GLUT-1 Deficiency Syndrome, epilepsy, and ID was admitted to the hospital with behavioral disturbances, including agitation and stereotyped hand movements. Infection, metabolic and electrolyte disturbances, and substance intoxication were ruled-out with laboratory workup. Episodes of mouthing words and swatting at the air were captured on electroencephalogram and had no epileptiform correlate. Psychiatry was consulted for psychosis. During the evaluation, the patient presented as euthymic, very concrete and cognitively limited, speaking in 2-3 word sentences. She would intermittently pause to make gestures and mouth words as though she was in an argument with someone. Still, she was able to return her attention to the conversation immediately when redirected. Stereotyped movements appeared consistent with popular TikTok trends which the patient was noted to watch. The patient had no history of formal cognitive testing. Her mother’s estimation was that she functioned at the level of an 8-year-old. However, focused questioning and observation suggested a developmental level of a toddler was more accurate.
Discussion: Even with a standardized approach, evaluation of psychosis is challenging. Symptoms which may appear bizarre in older children and adolescents may be appropriate for developmentally younger children. Examples include magical thinking, personification, mimicry, and the use of transitional objects. Good conceptualization of the patient’s developmental level is necessary for appropriate evaluation of such presentations, especially those with intellectual disability (Morgan, 2018). Additionally, awareness of current social media trends across the developmental age groups can be diagnostically useful (Siegel, 2020). This case describes a patient who engaged in mimicking popular social media trends and repetitive “conversations” to construct meaning and mastery over a stressful event.
Conclusion: Individuals with ID are at a risk of being misdiagnosed with psychotic disorders. It is important for clinicians determine a patient’s developmental level and evaluate accordingly.
References:
1. Morgan, V et al. Intellectual disability co-occurring with schizophrenia and other psychiatric illness: population-based study. The British Journal of Psychiatry. 2018; 193(5), 364-372.
2. Siegel, M et al. Practice Parameter for the Assessment and Treatment of Psychiatric Disorders in Children and Adolescents with Intellectual Disability. Journal of the American Academy of Child & Adolescent Psychiatry. 2020; 59: 468-496.
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: Despite widespread calls for culturally formulated updates to the DSM, racial and cultural bias remains a factor in psychiatric diagnosis. Decades of research has shown that African Americans and Latino Americans, in particular, are significant more likely than Caucasian Americans to be diagnosed with psychotic disorders. Additionally, individuals with intellectual disability may display "magical thinking," more commonly seen in chronologically and developmentally younger patients, that may be confused for psychosis. The case presented is of an African American female with intellectual disability who was mistakenly labeled as psychotic.

