Catatonia
(013) A Case of Catatonia due to Manganese Neurotoxicity from Total Parenteral Nutrition

Katherine Dickson, MD MPH
Fellow
NYU Langone
New York, New York
Katherine Dickson, MD MPH
Fellow
NYU Langone
New York, New York- JL
Justin Lewin, n/a
Consultation-Liaison Attending Psychiatrist
Psychiatry/Consult-Liaison/Bellevue Hospital
Long Island city, New York - JL
Justin Lewin, n/a
Consultation-Liaison Attending Psychiatrist
Psychiatry/Consult-Liaison/Bellevue Hospital
Long Island city, New York
Presenting Author(s)
Co-Author(s)
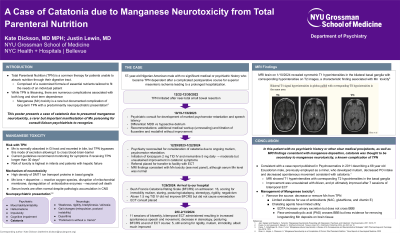
In considering potential etiologies of catatonia, MRI brain revealed symmetric T1 hyperintensities in the bilateral basal ganglia with corresponding hyperintensities on T2 weighted images, a characteristic finding associated with manganese toxicity (Khan, 2020). In this patient with no psychiatric history or other clear medical precipitants, as well as MRI findings consistent with manganese deposition, catatonia was thought to be secondary to manganese neurotoxicity, a known complication of TPN. References Jain, Sargam and Stephen J. Ferrando. “Manganese Neurotoxicity Presenting with Depression, Psychosis, and Catatonia”. Psychosomatics. 2011: 52:74-77 Khan, A., Hingre, J., Dhamoon, A. “Manganese Neurotoxicity as a Complication of Chronic Total Parenteral Nutrition.” Case Reports in Neurological Medicine. 2020 Peres, T., Schettinger, M., Chen, P. et al. “Manganese-induced neurotoxicity: a Review of its Consequences and Neuroprotective Strategies”. BMC Pharmacology and Toxicology. Nov 2016: 17(1)
Background: Total Parenteral Nutrition (TPN) is a common therapy for patients unable to absorb nutrition through their digestive tract. Patients on TPN receive a customized formula of essential nutrients to fit individual needs. While TPN is lifesaving, there are numerous complications associated with both long and short term dependence. Manganese toxicity is a rare but documented complication of long-term TPN with a predominantly neuropsychiatric presentation including mood and behavioral changes, cognitive dysfunction, and parkinsonism (Khan, 2020). We present a case of catatonia due to presumed manganese neurotoxicity, which is a rarer but very relevant manifestation of manganese poisoning for consult-liaison psychiatrists to recognize.
Case: This is the case of a 57-year-old Nigerian American male with no significant medical or psychiatric history who became TPN dependent after a complicated postoperative course for superior mesenteric ischemia. He developed mutism, blunted affect, and reduced oral intake about 3 months after TPN initiation. Psychiatry was consulted initially to evaluate for depression, however on exam his presentation was more consistent with catatonia, with Bush Francis Catatonia Rating Scale (BFCRS) of 20-23, scoring for mutism, withdrawal, stereotypy, catalepsy, grasp reflex, posturing, and vital sign instability. Response to lorazepam was significant but time-limited, and the patient was ultimately treated with 11 sessions of ECT resulting in improvement in spontaneous movement and speech.
Discussion: We discuss the association between manganese neurotoxicity and TPN and the mechanism of neuronal damage. We review the common neuropsychiatric manifestations of manganese toxicity, and review another case of catatonia presumed to be secondary to manganese poisoning (Jain, 2011). Lastly, we present options for management, the mainstay of which is removal of the underlying source (Peres, 2016).
Conclusion: As consult-liaison psychiatrists working with medically complex patients, some of whom are TPN dependent, it is important to recognize the numerous complications of this life-saving treatment. Because of its associated neuropsychiatric symptoms, manganese toxicity is an especially relevant complication for psychiatrists. Although less commonly documented than mood changes and parkinsonism, catatonia is a potential presentation which should be recognized and treated. While treatment relies primarily on removing the underlying exposure, managing the resultant neuropsychiatric effects- in this case catatonia- is critical for patient safety and quality of life.
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: While the vast majority of U.S. medical literature is based upon findings from individuals of European descent, his case describes a Black, Nigerian-American male with presumed manganese neurotoxicity. Additionally, world-wide, the most common route of exposure to excess manganese is environmental, specifically through inhalation, and is an occupational hazard associated with mining and welding jobs primarily in Central and South America (Jain, 2011). As increased numbers of individuals move to the US from Central and South America, manganese toxicity should be considered on the differential diagnosis with patients presenting with acute neuropsychiatric changes.

