Transplant Psychiatry and C-L Subspecialties
"I only wanted to help someone I love: A Tangled Tale In Living Donation
(205) I only wanted to help someone I love: A Tangled Tale In Living Donation

Vlad I. Velicu, MD
Fellow
The Mount Sinai Hospital
Kew Gardens, New York.jpg)
Shruti P. Mutalik, MD
Transplant and Consultation Liaison Psychiatrist, Mount Sinai Hospital
Icahn School of Medicine, Mount Sinai
New York, New York.jpg)
Jacob Appel, MD, DPAPA
Professor
Icahn School of Medicine at Mount Sinai
New York, New York
Omar Mirza, DO
Medical Director of Inpatient Psychiatry
NYC Health + Hospitals | Harlem
New York, New York- AY
Ambika Yadav, MD
Assistant Professor and Attending Psychiatrist
Mount Sinai Hospital
New York, New York
Presenting Author(s)
Co-Author(s)
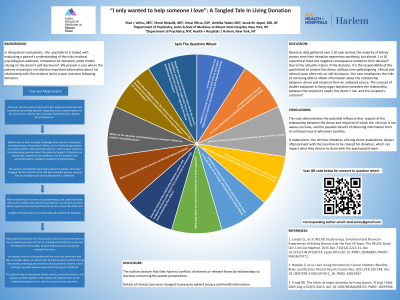
In living donor evaluations, the psychiatrist is tasked with evaluating a patient’s understanding of the risks involved, psychological readiness, and motivation for donation, while mostly relying on the donor’s self-disclosure (Truong et al., 2005). We present a case where the patient choosing to not disclose important information about his relationship with the recipient led to a poor outcome following donation. A 35 year old man with a history of major depressive disorder and borderline personality disorder requested to be a kidney donor for his uncle. The patient consistently expressed a desire to donate, but never divulged the fact that his uncle had been sexually abusive towards him for multiple years during the patient’s childhood. He was initially deemed a moderate psychosocial risk for donation and referred to individual psychotherapy. After completing six months of psychotherapy, the patient was cleared to donate; however, following donation, he expressed regret about his decision and disclosed the history of abuse to the transplant psychiatrist. Based on data gathered over a 50 year period, the majority of kidney donors view their donation experience positively, but almost 1 in 10 reported at least one negative consequence related to their decision (Jacobs et al., 2015). Due to the altruistic nature of the decision, it is the responsibility of the psychiatrist to protect the donor, without over pathologizing. Clinical and ethical issues often rely on self-disclosure. Our case emphasizes the risks of not being able to obtain information about the relationship between donor and recipient from an unbiased source. The concept of double equipoise in living organ donation considers the relationship between the recipient’s needs, the donor’s risk, and the recipient’s outcome (Nadalin et al., 2021). We raise the question of whether the nature of the relationship between donor and recipient can risk additional harm to the donor. This case also raises the question of whether there would be any circumstance under which the donation should have been approved had the information regarding the abuse perpetrated been known. This case demonstrates the potential influence that aspects of the relationship between the donor and recipient of which the clinician is not aware can have, and the possible benefit of obtaining information from an unbiased source whenever possible. It underscores the intrinsic limitation of living donor evaluations: donors often present with the incentive to be cleared for donation, which can impact what they choose to share with the psychosocial team. Some details of the case were changed to protect patient privacy. Jacobs CL, et al. RELIVE Study Group. Emotional and Financial Experiences of Kidney Donors over the Past 50 Years: The RELIVE Study. Clin J Am Soc Nephrol. 2015 Dec 7;10(12):2221-31. doi: 10.2215/CJN.07120714. Epub 2015 Oct 13. PMID: 26463883; PMCID: PMC4670771. Nadalin S, et al. Liver Living Donation for Cancer Patients: Benefits, Risks, Justification. Recent Results Cancer Res. 2021;218:135-148. doi: 10.1007/978-3-030-63749-1_10. PMID: 34019167. Truog RD. The ethics of organ donation by living donors. N Engl J Med. 2005 Aug 4;353(5):444-6. doi: 10.1056/NEJMp058155. PMID: 16079366.
Background:
Case:
Discussion:
Conclusion:
References:
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: We will discuss the importance of equity in the transplant evaluation process and the fact that a lack of diversity could impact donor evaluation given that people tend to believe some people more than others because of shared identity, race, or gender. Our submission also has a diverse group of authors: three of the authors were born and raised outside of the United States (in India and Romania), one of the authors is a United States Military Veteran, the authors are of mixed genders, and the presenting author is a trainee (PGY-4 Psychiatry Resident).

