Neurocognitive Disorders and Neuropsychiatry
(089) Down the Wrong Rabbit Hole: Unraveling Alzheimer's Disease when Encephalitis is Suspected

Jennie Vyas
Medical Student
University of Miami Miller School of Medicine
Miami, Florida.jpg)
Maria Rueda Lara, FACLP, FAPA
Assistant Professor of Psychiatry
University of Miami. Sylvester Comprehensive Cancer Center
Miami, Florida
Zelde Espinel, MD
Psychiatrist
University of Miami
Miami, Florida
Presenting Author(s)
Co-Author(s)
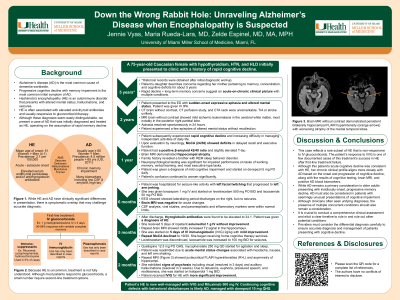
Background: Alzheimer's disease (AD) is the most common cause of dementia worldwide, characterized by progressive cognitive decline with memory impairment as the most common initial symptom (Scheltens, 2021). Hashimoto's encephalitis (HE), an autoimmune disorder that presents with altered mental status, hallucinations, and seizures, is often associated with elevated anti-thyroid antibodies and usually responsive to glucocorticoid therapy (Chaudhuri, 2023). Although these diagnoses seem easily distinguishable, we present a case of AD that was initially diagnosed and treated as HE, operating on the assumption of rapid memory decline.
Case: A 75-year-old Caucasian female presented with a history of rapid cognitive decline. Two years ago, patient presented to a hospital for sudden-onset expressive aphasia. Comprehensive workup, including neurological exam and brain MRI, was negative. Although the aphasia resolved spontaneously within 24 hours, the family indicated that patient subsequently experienced rapid cognitive decline and increasing difficulty in managing independent activities of daily life. Upon evaluation by neurology, MoCA showed deficits in delayed recall and executive function. Patient had a positive beta-amyloid 42/40 ratio and slightly elevated T-tau. Brain MRI demonstrated hippocampal atrophy. Family history revealed a brother with REM sleep behavior disorder. Neuropsychological testing was significant for impaired performance on tasks of working memory, verbal learning, and most executive type tasks. Patient was given a diagnosis of mild cognitive impairment.
One year later, patient experienced a seizure with left facial twitching and arm jerking. She was hospitalized and extensive workup was performed. EEG showed lateralizing period discharges on the right, but no seizures were seen. CSF analysis was within normal limits. Upon discharge, patient was found to have elevated thyroglobulin antibodies. She was given a diagnosis of HE and received 5 days of IV steroids without improvement. She then was treated with IVIG over 5 days with minimal change. Repeat brain MRI showed decreased hippocampal volume and medial temporal lobe atrophy. Historical records were obtained showing that the patient had subjective memory complains dating back 5 years. When the totality of findings was reconsidered in the context of chronic memory loss, a diagnosis of Alzheimer’s disease was given.
Conclusions: While AD remains a primary consideration in older adults presenting with insidiously-onset, progressive memory decline, AD must also be considered in patients with seemingly unusual presentations of cognitive impairment. It is crucial for clinicians to conduct a comprehensive clinical assessment and elicit a clear timeline to rule out other potential conditions. The diagnosis of HE requires exclusion of other causes of encephalopathies and encephalitis. Despite the presence of thyroid antibodies, this patient's clinical profile aligns more closely with AD than HE based on the onset and progression of cognitive decline, along with the results of cognitive testing, brain MRI, and positive AD blood biomarkers. Clinicians must consider the differential diagnosis carefully to ensure accurate diagnosis and management of patients presenting with cognitive decline.
References:
Chaudhuri J, Mukherjee A, Chakravarty A. Hashimoto's Encephalopathy: Case Series and Literature Review. Curr Neurol Neurosci Rep. 2023;23(4):167-175.
Scheltens P, De Strooper B, Kivipelto M, et al. Alzheimer's disease. Lancet. 2021;397(10284):1577-1590.
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: This case emphasizes the need for healthcare providers to recognize the diverse range of health conditions that may affect older individuals, including comorbidities and age-related changes. Ensuring equitable treatment for older adults involves addressing age-related biases and stereotypes that may impact the quality of care they receive. Recognizing the intersectionality of age and gender, healthcare providers must consider how gender identity might shape healthcare experiences. Older women may encounter distinct health challenges and disparities relative to men. Healthcare providers should be attentive to the needs of older adult women, including addressing gender-specific health concerns and providing suitable care and support.

