Cardiology
(008) Demographic and Clinical Characteristics of Genetic Variants (KCNQ1, KCNH2, SCN5A, KCNE1, KCNJ2) of Long QT Syndrome and Vulnerability to QTc Prolongation with Psychotropics: A Case Report and Systematic Review of the Literature
- VD
Vanessa Dang, MD (she/her/hers)
Psychiatrist
Mayo Clinic - Rochester
Rochester, Minnesota - VD
Vanessa Dang, MD (she/her/hers)
Psychiatrist
Mayo Clinic - Rochester
Rochester, Minnesota .jpg)
David C. Fipps, DO
Assistant Professor of Psychiatry
Mayo Clinic
Rochester, Minnesota.jpg)
David C. Fipps, DO
Assistant Professor of Psychiatry
Mayo Clinic
Rochester, Minnesota
Presenting Author(s)
Co-Author(s)
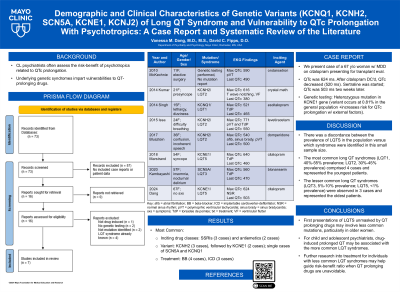
Background: Consultation-liaison psychiatrists often assess the risk-benefit of psychotropics related to QTc prolongation. Though genetic variants impart vulnerabilities to QTc prolongation, limited characterization of presentations exist in the literature, and clinical guidance is lacking when faced with long QT syndromes (LQTS). We present an exemplary case and systematic review of case reports describing the demographic and clinical characteristics of genetic vulnerabilities to QTc prolongation and summarize considerations for psychotropic use in these scenarios.
Case: A 67 year old woman with major depressive disorder on citalopram presented for transplant evaluation and was found to have a prolonged QTc (624 ms). After citalopram discontinuation, QTc decreased (520 ms) the following day. Sertraline was started; QTc was 503 ms two weeks later. Genetic testing identified a heterozygous mutation in the KCNE1 gene. Genetic counseling indicated that this variant occurs at 0.81% in the general population and increases risk for QTc prolongation with external factors.
Methods: We systematically reviewed the literature. Inclusion criteria: case reports of drug-induced QTc prolongation revealing underlying genetic mutations (“group 1”), or patients with known LQTS requiring psychotropics (“group 2”). Exclusion criteria: non-English, no genetic component. Extracted variables: age, gender, genetic variant, pre-QTc, post-QTc, EKG findings, comorbid diagnoses, presenting symptoms, and additional interventions.
Results: We identified 12 cases (10 female). Group 1 (8 cases): most common inciting drug classes: SSRIs (3 cases) and antiemetics (2 cases). Other classes occurred in isolation: antipsychotics, antiepileptics, and stimulants. All cases developed ventricular tachycardia, 4 went into TdP, and QTc ranged from 540 to 771 ms. After drug discontinuation, QTc decreased to < 500 ms in 5 cases. Most common variant: KCNH2 (3 cases), followed by KCNE1 (2 cases). There were isolated cases of SCN5A and KCNQ1. One patient’s mutation was not reported despite genetic testing. Group 2 (4 cases): all 4 patients had different psychiatric presentations. Mutations were not reported in 2 patients. The other 2 had KCNJ2 or KCNH2 mutations. Two had cardiac defibrillators. One patient did not have a post-exposure QTc recording, but ICD discharges were monitored.
Discussion: Gene mutations affecting cardiac potassium or sodium channel function can cause LQTS. KCNE1, less commonly associated with LQTS, was identified in two cases in our series, both unmasked by psychotropics. Psychiatric medication management for patients with LQTS was accomplished with QTc or ICD monitoring. We will discuss safety profiles of psychotropics and clinical management strategies in such cases with genetic vulnerabilities.
Conclusion: Consolidating knowledge of interactions between psychotropics and genetic susceptibilities to QTc prolongation may help direct clinical decisions. Lesser known LQTS genetic mutations should be included in risk-benefit assessments.
References:
Itoh H, Sakaguchi T, Ding WG, et al. Latent genetic backgrounds and molecular pathogenesis in drug-induced long-QT syndrome. Circ Arrhythm Electrophysiol. 2009;2(5):511-523. doi:10.1161/CIRCEP.109.862649
Lane CM, Giudicessi JR, Ye D, et al. Long QT syndrome type 5-Lite: Defining the clinical phenotype associated with the potentially proarrhythmic p.Asp85Asn-KCNE1 common genetic variant. Heart Rhythm. 2018;15(8):1223-1230. doi:10.1016/j.hrthm.2018.03.038
Lankaputhra M, Voskoboinik A. Congenital long QT syndrome: a clinician's guide. Intern Med J. 2021;51(12):1999-2011. doi:10.1111/imj.15437
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: Our poster on congenital long QT syndrome has implications for inclusion of a rare disease that does not usually gain much attention from the psychiatric field. In addition, long QT syndromes are more common in the African American population and in women (who also have a higher mortality rate), thus this data allows for a more robust understanding of disease processes in underserved and under-researched populations.

