Training, Education, Mentorship, and Career Development
(197) Decision Making Capacity Assessment: Efficacy and Satisfaction of an Iterative Curriculum
.jpg)
Brittany Goldstein, MD (she/her/hers)
CL Psychiatry Fellow
Northwestern University
Chicago, Illinois- CA
Cara Angelotta, MD
Vice Chair for Education, Residency Program Director
Northwestern University Feinberg School of Medicine
C, Illinois
Presenting Author(s)
Co-Author(s)
INTRODUCTION
The assessment of patients’ decision-making capacity (DMC) is a critical skill for all physicians, yet the literature describes a lack of preparation, comfort, and competence amongst practicing physicians. (1-2) While physicians often turn to CL psychiatrists as the experts in DMC, many medical students will go on to work in non-academic settings without access to psychiatric consultation. Thus, we must prepare future physicians early to achieve mastery in this skill. CL psychiatrists play a vital role in educating healthcare students on DMC skills. There is no standardized method for teaching or evaluating DMC assessment in undergraduate medical education. The limited literature supports the use of active learning for such communication skills. (3-5) We present an iterative DMC curriculum and communication checklist.
METHODS
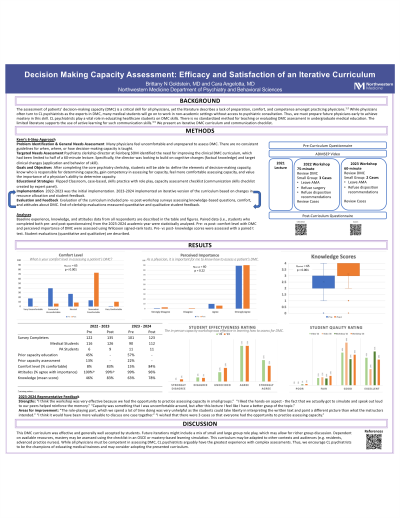
We developed a DMC course within the core psychiatry clerkship curriculum using Kern's six-step approach. A capacity assessment checklist was created by an expert panel. The course utilized a flipped classroom model: students complete a self-directed online module followed by an in-person workshop. We evaluated the efficacy of this curriculum by comparing pre-/posttest changes in knowledge and comfort in DMC assessment. The first iteration of this course was implemented in 2022-2023. In response to student feedback and resource availability, an updated iteration was implemented in 2023-2024 and the outcomes from this updated iteration will be presented here.
RESULTS
Data from the first 8 blocks of the 2023-2024 academic year are presented here, which will be updated once the full year of data is available. Of the 54 students who completed the pre-test, 63% previously received DMC education and 20% had participated in a DMC assessment. Pre- vs post- course data were as follows: mean knowledge scores improved (2.60 to 3.25 out of 4 points); comfort levels increased from 19% to 88% of students feeling comfortable in assessing capacity. Of students who completed the end-of-course evaluations, 67.3% agreed or strongly agreed that the capacity curriculum was effective at teaching this skill. The majority of students evaluated the quality of the online module and workshop as “good” or “excellent” (mean rating: 3.09 and 3.13, respectively, on a 4-point scale).
DISCUSSION
This DMC curriculum was effective and generally well accepted by students. Future iterations might include a mix of small and large group role play, which may allow for richer group discussion. Dependent on available resources, mastery may be assessed using the checklist in an OSCE or mastery-based learning simulation. This curriculum may be adapted to other contexts and audiences (e.g. residents, advanced practice nurses). While all physicians must be competent assessing DMC, CL psychiatrists arguably have the greatest experience with complex assessments. Thus, we encourage CL psychiatrists to be the champions of educating medical trainees, and may consider adopting the presented curriculum.
REFERENCES
1. Young G, et al. (2018) NZ Med J.
2. Seyfried L, et al. (2013) Psychosomatics.
3. Bishop et al. (2021) Med Sci Educ.
4. Frank, A. (2015) MedEdPORTAL.
5. Gillis AE, et al. (2015) Postgrad Med J.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: By improving accessibility of high quality medical education for critical skills such as decision making capacity we promote ethical practice of medicine among future physicians. This also provides physicians with the skills to uphold patient autonomy and equity based on objective and equitable assessment for all patients.

