Neurocognitive Disorders and Neuropsychiatry
(088) Converting Weakness into Strength: Rapid Resolution of Functional Neurological Symptom Disorder with Intravenous Lorazepam

Amir A. Mohammadzadeh, MD
Psychiatry Resident
Vanderbilt University Medical Center
Nashville, Tennessee.jpg)
Jo E. Wilson, MD, PhD, MPH
Assistant Professor
Vanderbilt University
Nashville, Tennessee.jpg)
Jonathan Smith, MD
Medical Director, Fellowship Director
Vanderbilt University Medical Center
Nashville, Tennessee
Presenting Author(s)
Co-Author(s)
Background/Significance: Functional neurological symptom disorder (FNSD), also known as conversion disorder, is defined as altered motor or sensory function incompatible with another recognized disorder resulting in clinically significant distress (APA, 2022). Its incidence is 4-12 per 100,000 annually and it accounts for 6% of outpatient neurology encounters (Carson, 2016). Nevertheless, it remains a resource-intensive diagnostic and treatment challenge for clinicians and patients alike, with charges for emergency department (ED) and inpatient care of FNSD estimated to be over $1.2 billion per year (Stephen, 2021). Here we present a case of FNSD which rapidly resolved after intravenous (IV) lorazepam administration.
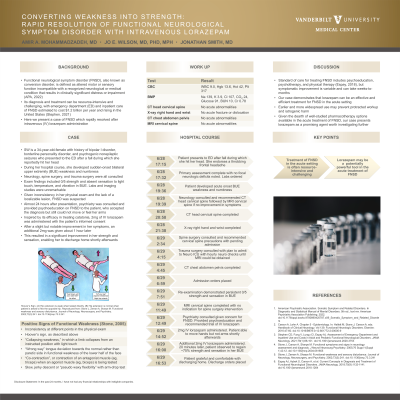
Case: SW is a 34-year-old female with a history of borderline personality disorder and psychogenic nonepileptic seizures who presented to the ED after a fall. During her ED course, she developed sudden-onset bilateral upper extremity (BUE) weakness and numbness. Neurology, spine surgery, and trauma surgery were consulted. Exam findings included 0/5 strength and absent sensation to light touch, temperature, and vibration in BUE. Chest x-ray, bilateral hand x-ray, CT head cervical spine, CT chest abdomen pelvis, and MRI cervical spine were unremarkable. Labs were within normal limits. Given inconsistency in her symptoms and the lack of a localizable lesion, FNSD was suspected. 24 hours after presentation, psychiatry was consulted and provided psychoeducation on FNSD to the patient, who accepted the diagnosis but remained unable to move or feel her arms. Inspired by its efficacy in treating catatonia, 2mg of IV lorazepam was administered with the patient’s informed consent. After slight but notable improvement in her symptoms, an additional 2mg was given an hour later. To the patient’s gratification, this resulted in an approximately 75% improvement in her strength and sensation, enabling her to discharge home shortly afterwards.
Discussion: The mainstay of treating FNSD includes psychoeducation, psychotherapy, and physical therapy (Espay, 2018), though symptomatic improvement is variable and can take weeks-to-months. Our case demonstrates that lorazepam can be an effective and efficient treatment for FNSD in the acute ED setting. Earlier and more widespread use may prevent protracted workup and iatrogenic harm. Given the dearth of well-studied pharmacotherapy options available in the acute treatment of FNSD, our case presents lorazepam as a promising agent worth investigating further.
Conclusion/Implications: Lorazepam can be a potentially powerful tool in the consult-liaison psychiatrist’s armamentarium for the acute treatment of FNSD.
References:
1. American Psychiatric Association. Somatic Symptom and Related Disorders. In: Diagnostic and Statistical Manual of Mental Disorders. 5th ed., text rev. American Psychiatric Association Publishing; 2022. doi:10.1176/appi.books.9780890425787.x09_Somatic_Symptom_and_Related_Disorders
2. Carson A, Lehn A. Chapter 5 - Epidemiology. In: Hallett M, Stone J, Carson A, eds. Handbook of Clinical Neurology. Vol 139. Functional Neurologic Disorders. Elsevier; 2016:47-60. doi:10.1016/B978-0-12-801772-2.00005-9
3. Stephen CD, Fung V, Lungu CI, Espay AJ. Assessment of Emergency Department and Inpatient Use and Costs in Adult and Pediatric Functional Neurological Disorders. JAMA Neurol. 2021;78(1):88-101. doi:10.1001/jamaneurol.2020.3753
4. Espay AJ, Aybek S, Carson A, et al. Current Concepts in Diagnosis and Treatment of Functional Neurological Disorders. JAMA Neurol. 2018;75(9):1132-1141. doi:10.1001/jamaneurol.2018.1264
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: Patients with FNSD can face inequity in treatment from healthcare providers due to suspicions that their neurologic symptoms may be feigned. In addition to being invalidating, such bias can prevent FNSD patients from accessing the care they need. Our study depicts a case in which our patient’s symptoms were validated not only by being given a diagnosis, but also by being treated. In addition to providing hope for a historically challenging condition to treat, our case emphasizes the importance of equal care and inclusivity for all patients presenting to the ED – no matter how atypical their symptoms may be.

