Training, Education, Mentorship, and Career Development
(201) Teaching to the “Last Mile” of Health Care Delivery: A Collaborative Care Implementation Rotation for Psychiatry Residents
- JW
Jessie Whitfield, MD, MPH
Assistant Professor
University of Washington School of Medicine
Seattle, Washington 
Joseph Baldwin, MD
Psychiatrist
Loyola University Medical Center
Chicago, Illinois
Presenting Author(s)
Co-Author(s)
Background:
With a crisis in access to mental health care, the successful provision of psychiatric care becomes increasingly dependent on navigating inefficient systems. This is especially true for those patients with increased barriers, including those from low socioeconomic backgrounds and racial/ethnic minorities, which collaborative care programs have shown to be effective in improving treatment. (Hu J et al 2020) Teaching residents about systems factors that impact patient care, or how to navigate ‘the last mile’ of mental health care delivery, can improve their effectiveness as clinicians and prepare them with the skills to lead meaningful systems-level change (Castillo E et al 2020). Evidence shows that psychiatry trainees are interested in systems-based practice knowledge, but often identify it as a gap in their training. (Fried J et al 2014).
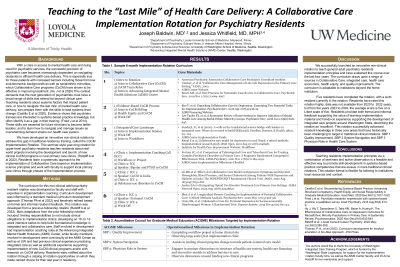
We have developed an innovative non-clinical rotation to address this educational gap, called the Collaborative Care Implementation Rotation. This seminar-style year-long rotation for upper-level psychiatry residents teaches about real-world projects involving the development and launch of Collaborative Care programs in rural primary care clinics. (Ratzliff A et al 2022). Residents learn a systematic approach to the implementation of Collaborative Care and work with faculty to support local primary care clinics through phases of the implementation process.
Methods:
We used a six-step approach to adapt the curriculum for this rotation from our integrated care training fellowship program (Thomas P et al 2015). Iterative feedback sessions were conducted informally with residents to tailor the rotation to their interest and update the curriculum overtime. Resident feedback was obtained formally through residency evaluations. Canvas was used for publication of the curriculum.
Results:
The Collaborative Care Implementation Rotation launched in 2020, with six residents completing the rotation and an overall higher than average rotation rating. The rotation includes a three-month implementation ‘intensive’ that builds basic knowledge in implementation, as well as several regularly returning faculty who provide lectures on specialty topics. Residents have assisted in the implementation of Collaborative Care at five primary care clinics.
Discussion
Teaching residents in a seminar-style rotation with supported observation of the implementation process is both a feasible and effective way to deliver systems-based practice education. We review potential adaptations to the curriculum to make it more generalizable to other institutions.
Conclusion:
To combat current issues in the mental health care delivery climate, residency programs should improve training in systems-based practice. This rotation demonstrates an effective approach to meeting this educational need.
References
Castillo, E et al. Reconsidering Systems-Based Practice: Advancing Structural Competency, Health Equity, and Social Responsibility in Graduate Medical Education. Academic medicine. (2020)95(12), 1817–1822.
Fried JL et al. Psychiatry residents' experiences with systems-based practice: a qualitative survey. Acad Psychiatry. (2014)Aug;38(4):414-9.
Hu J, et al. The Effectiveness of Collaborative Care on Depression Outcomes for Racial/Ethnic Minority Populations in Primary Care: A Systematic Review. Psychosomatics. (2020)Nov-Dec;61(6):632-644.
Ratzliff ADH et al. Development and Implementation of an Integrated Care Fellowship. J Acad Consult Liaison Psychiatry. (2022)May-Jun;63(3):280-289.
Thomas, PA et al (2015). Curriculum development for medical education: A six-step approach. Johns Hopkins University Press.
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: Recognizing and addressing systemic inequities in health care requires stepping back and examining the systems in which we work, function, and live as physicians and humans. This non-clinical rotation provides a space for psychiatry trainees to engage in this broader systems-based practice work, including a specific module called ‘health care inequities’ that examines the effectiveness of integrated care in addressing some (though not all) aspects driving health care inequities.

