Transplant Psychiatry and C-L Subspecialties
(229) Tacrolimus-induced Catatonia after Organ Transplantation: Two Case Reports
- JL
Jamie Lee, MD
Clinical Assistant Professor
Thomas Jefferson University Hospital
Philadelphia, Pennsylvania 
Paulina Khodak, DO
Consultation & Liaison Psychiatry Fellow Physician
Thomas Jefferson University Hospital
Philadelphia, Pennsylvania- KC
Keira Chism, MD
Director CL Division, Chief Transplant Psychiatry
Jefferson
Philadelphia, Pennsylvania
Presenting Author(s)
Co-Author(s)
Background:
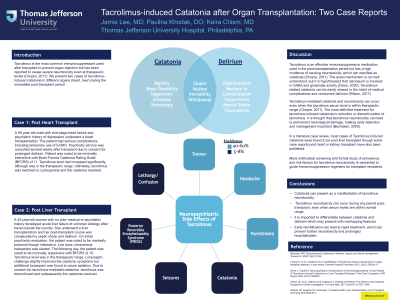
Tacrolimus is the most common immunosuppressant used after transplant to prevent organ rejection, but has been reported to cause severe neurotoxicity even at therapeutic levels (Chopra, 2011). We present two cases of tacrolimus-induced catatonia in different organs during the immediate post-transplant period. Cases: Case 1 A 65-year-old male with end-stage heart failure and psychiatric history of depression underwent a heart transplantation. The patient had serious complications including temporary use of ECMO. Psychiatry service was consulted several weeks after transplant due to concern for prolonged delirium. Patient was noted to be minimally interactive with Bush-Francis Catatonia Rating Scale (BFCRS) of 11. Tacrolimus level was in the therapeutic range. Ultimately, tacrolimus was switched to cyclosprine and the catatonia resolved. Case 2 A 43-year-old woman with no prior medical history developed acute liver failure of unknown etiology after travel outside the country. She underwent liver transplantation and her post-transplant course was complicated by septic shock and delirium. On initial psychiatric evaluation, the patient was noted to be markedly paranoid, though interactive. Low dose haloperidol was started. The following day, the patient was noted to be minimally responsive with BFCRS of 15. Lorazepam challenge slightly improved the catatonic symptoms but additional lorazepam caused sedation. Due to concern for tacrolimus-mediated catatonia, tacrolimus was discontinued and subsequently the catatonia resolved. Tacrolimus is an effective immunosuppressive medication used in the post-transplantation period, but has a high incidence of causing neurotoxicity, which can manifest as catatonia (Chopra, 2011). The exact mechanism is not well understood, but it is hypothesized that calcineurin is involved in GABA and glutamate activity (Davis, 2020). Tacrolimus-related catatonia can be easily missed in the midst of medical complications and concurrent delirium (Wilson, 2017). Also, tacrolimus-mediated catatonia and neurotoxicity can occur even when the tacrolimus serum level is within therapeutic range, adding to the diagnostic challenge (Chopra, 2011). The most definitive treatment for tacrolimus-induced catatonia is reduction or discontinuation of tacrolimus. It is thought that tacrolimus neurotoxicity can lead to permanent neurological damage, making early detection and management important (Bechstein, 2000). Additionally, more methodical screening and formal study of prevalence and risk factors for tacrolimus neurotoxicity is warranted to guide immunosuppression regimens for transplant recipients. Catatonia can present as a manifestation of tacrolimus neurotoxicity. Tacrolimus neurotoxicity should be considered when patients on tacrolimus have a mental status change, even if the serum tacrolimus level is within the normal range. Early identification can lead to rapid treatment, which can prevent further neurotoxicity and prolonged hospitalization. Bechstein WO. Neurotoxicity of calcineurin inhibitors: impact and clinical management. Transpl Int. 2000;13(5):313-26. Chopra A, et al.: Catatonia as a manifestation of tacrolimus-induced neurotoxicity in organ transplant patients: a case series. General Hospital Psychiatry 2012; 34(2): 209.e9–11. Davis L, Tripathi S: Neuropsychiatric Complications of Immunosuppressants: A Case Report of Tacrolimus-Induced Catatonia in a Liver Transplant Recipient. Prim Care Companion CNS Disord 2020; 22(1):19I02481 Wilson JE, et al.: Delirium and Catatonia in Critically Ill Patients: The Delirium and Catatonia Prospective Cohort Investigation. Crit Care Med. 2017 Nov;45(11):1837-1844.
Discussion:
Conclusion:
References:
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: Racial and socioeconomic disparities unfortunately remain an issue impacting access to transplant for many marginalized groups, and these can extend into post-transplant care. In a study conducted by Lehr and colleagues, it was found that black patients had a demonstrable disadvantage in post–lung transplant survival, as did recipients who received lungs from donors residing in the least resourced neighborhoods. Therefore, clinicians must not only be educated about post-transplant complications, we must also be vigilant for disparities in post-transplant care that are related to racial and socioeconomic differences.

