Psycho-Oncology and Palliative Care
(124) Suicidal Ideation, End of Life, or Personality? A case series of voluntarily stopping eating and drinking.

Stacey Roll, DO (she/her/hers)
Psychiatry Resident
Cleveland Clinic
Cleveland, Ohio- NN
Nona Nichols, MD
Staff
Cleveland Clinic
Cleveland, Ohio
Presenting Author(s)
Co-Author(s)
Suicidal ideation, end of life, or personality? A case series of voluntarily stopping eating and drinking.
Roll, S., Nichols, N.
Background:
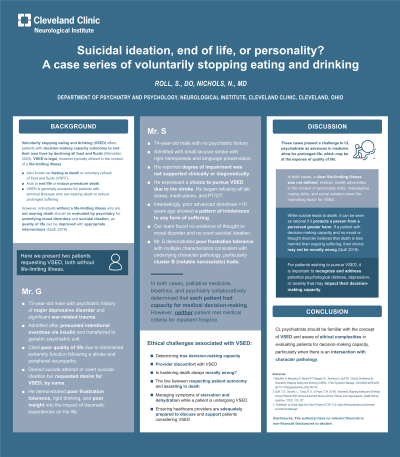
Voluntarily stopping eating and drinking (VSED) offers patients with decision-making capacity autonomy to end their own lives by declining all food and fluids (Wenchkin, 2023). VSED is generally accepted for patients with terminal illnesses. However, individuals without a life-limiting illness who are not actively dying should be evaluated by psychiatry for underlying mood disorders and suicidal ideation, as quality of life can be improved with appropriate interventions (Quill, 2018). Here we present two patients requesting VSED, both without life-limiting illness.
Cases:
Mr. S is a 74-year-old male with no psychiatric history found to have small lacunar stroke with right hemiparesis and language preservation. His reported degree of impairment was not supported clinically or diagnostically; however, he expressed a choice to pursue VSED because of his stroke. Our team found no evidence of thought or mood disorder and no overt suicidal ideation. However, Mr. S demonstrated poor frustration tolerance with multiple characteristics consistent with underlying character pathology, particularly cluster B (notable narcissistic) traits.
Mr. G is a 73-year-old male with a psychiatric history of major depressive disorder and significant war-related trauma admitted after presumed intentional overdose via insulin and transferred to our geriatric psychiatric unit. Patient cited poor quality of life due to diminished extremity function following a stroke and peripheral neuropathy. However, he denied suicide attempt or suicidal ideation but expressed desire for VSED. Similar to Mr. S, psychiatry found that patient demonstrated poor frustration tolerance, rigid thinking, and poor insight into the impact of traumatic experiences on his life.
In both cases, palliative medicine, bioethics, and psychiatry collaboratively determined that each patient had capacity for medical decision-making. However, neither patient met medical criteria for hospice.
Discussion:
These cases present a challenge to CL psychiatrists as advances in medicine allow for prolonged life, which may be at the expense of quality of life. In both cases, a clear life-limiting illness was not defined. Instead, health adversities in the context of personality traits, maladaptive coping skills, and social isolation were the motivating factor for VSED. We will review the concept of VSED and will examine the ethical challenges of evaluating similar patients for decision-making capacity particularly those with underlying character pathology.
Conclusion:
CL psychiatrists should be familiar with the concept of VSED and aware of ethical complexities in evaluating patients for decision-making capacity, particularly when there is an intersection with character pathology.
References:
1. Wechkin H, Macauley R, Menzel PT, Reagan PL, Simmers N, Quill TE. Clinical Guidelines for Voluntarily Stopping Eating and Drinking (VSED). J Pain Symptom Manage. 2023;66(5):e625-e631. doi:10.1016/j.jpainsymman.2023.06.016
2. Quill, T. E., Ganzini, L., Truog, R. D., & Pope, T. M. (2018). Voluntarily Stopping Eating and Drinking Among Patients With Serious Advanced Illness-Clinical, Ethical, and Legal Aspects. JAMA internal medicine, 178(1), 123–127. doi:10.1001/jamainternmed.2017.6307
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: Voluntarily stopping eating and drinking (VSED) offers patients with decision-making capacity, autonomy to end their own lives by declining all food and fluids. VSED could be implemented in any individual with decision-making capacity and a life-limiting illness, thus could apply to marginalized groups. However, no research/evidence exists on this clinical topic and its intersection with historically marginalized groups likely due to the limited research on the clinical topic overall and it's overlap with psychiatry. We recommend further research to include inclusion of historically marginalized groups to further advance health outcomes.

