Catatonia
(031) Sometimes there's no place like home: an illustrative case for the outpatient management of catatonia

Connor Hoch, MD
Consultation-Liaison Psychiatry Fellow, PGY-5
Columbia University/New York Presbyterian Hospital
New York, New York- SQ
Seema Quraishi, MD
Division Chief and Fellowship Program Director, Consultation-Liaison Psychiatry
Mount Sinai Beth Israel
New York, New York - AS
Ashley Sterchele, MD (she/her/hers)
Medical Director of Integrative Outpatient Services and Associate Program Director
Mount Sinai Beth Israel, New York
Co-Author(s)
Co-Author(s)
Presenting Author(s)
Background/Significance:
With its associated morbidity and mortality, catatonia is often considered a disease of inpatient diagnosis and management (Sienart, 2014; Ferrafiat 2024); however, psychiatric admission can be a distressing or even traumatic experience to those hospitalized (Martinaki, 2021). For select patients, an outpatient model for diagnosing and treating catatonia may represent a more person-centered approach, optimizing autonomy and preservation of usual routine while minimizing unintended harm that may result from hospitalization.
Case:
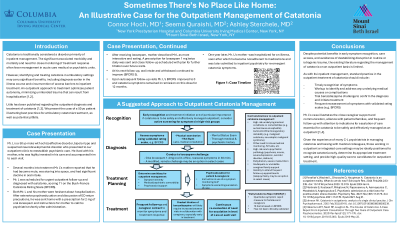
A 50-year-old man with schizoaffective disorder, bipolar type and suspected neurodevelopmental disorder presented to our outpatient clinic to reestablish care following a lapse in treatment. Several months into a gradual re-titration of his antipsychotic, his mother reported that he had become mute, stared purposelessly for prolonged periods, and had significant decline in oral intake. Upon urgent return evaluation, he scored 11/23 on the Bush-Francis Catatonia Rating Scale (BFCRS) and a diagnosis of catatonia was established.
Both the patient and his family were hesitant regarding the prospect of hospitalization. Considering the close support and monitoring provided by his mother, after careful discussion of risks and benefits, the patient was sent home with 2 mg of oral lorazepam with instructions for family to report any changes in his symptoms immediately following administration. His mother described substantial improvement in his catatonia symptoms after receiving lorazepam, and he was prescribed lorazepam 1 mg twice daily with close follow-up. Over subsequent visits in the ensuing weeks his catatonia resolved, and lorazepam was continued at the same dose with frequent follow-up.
Discussion:
While literature regarding the management of catatonia in the outpatient setting is sparse, this case illustrates several principals identified in the existing literature as essential to the safe evaluation and treatment of catatonia in the outpatient setting, including its prompt recognition, conducting a trial benzodiazepine induction, frequent reevaluation of symptoms, and extensive psychoeducation and collaboration with family or caregivers (Ferrafiat, 2024). We review the current literature on the outpatient management of catatonia, discuss its potential whole person benefits, and propose the unique skills C-L psychiatrists may bring to its management in this setting.
Conclusion/Implications:
For patients without life-threatening symptoms or comorbidities and with the appropriate psychosocial support, the diagnosis and management of catatonia on an outpatient basis may be considered as a lifestyle-preserving alternative to the typical inpatient setting of care. C-L psychiatrists practicing in outpatient settings may be especially well-poised to identify catatonia early and navigate the nuances of its management outside of the hospital.
References:
[1] Sienaert P, Dhossche DM, Vancampfort D, De Hert M, Gazdag G. A clinical review of the treatment of catatonia. Front Psychiatry. 2014 Dec 9;5:181. doi: 10.3389/fpsyt.2014.00181. PMID:25538636.
[2] Ferrafiat V, Wachtel L, Dhossche D, Hauptman A. Catatonia is an outpatient reality. What do we do now? Schizophr Res. 2024 Feb;264:233-235. doi: 10.1016/j.schres.2023.12.019. Epub 2024 Jan 6. PMID:38183961.
[3] Martinaki S, Kostaras P, Mihajlovic N, Papaioannou A, Asimopoulos C, Masdrakis V, Angelopoulos E. Psychiatric admission as a risk factor for posttraumatic stress disorder. Psychiatry Res. 2021 Nov;305:114176. doi: 10.1016/j.psychres.2021.114176. Epub 2021 Aug 21. PMID:34455217.
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: Patients of color are more likely to be psychiatrically hospitalized than their non-Hispanic White counterparts, and Black patients have been found to be overrepresented among an inpatient sample of those diagnosed with catatonia. Given these findings and the traditional inpatient setting of catatonia management, minority patients with catatonia may be likelier to be hospitalized psychiatrically, an experience that may be traumatic and potentially contributory to perceived lack of freedom or structural powerlessness in historically marginalized groups. For appropriately selected candidates, the outpatient management of catatonia may further equity and inclusion by reducing disparities in psychiatric hospitalization.

