Psychopharmacology and Toxicology
(153) Working together: Effective interdisciplinary collaboration to identify desvenlafaxine-induced burning mouth syndrome.

John Weller, MD
PGY3
Northwell Health
Port Jefferson, New York
John Weller, MD
PGY3
Northwell Health
Port Jefferson, New York
Mehgan Oswald, DMD, MD
Resident
Northwell Mather Hospital
Port Jefferson, New York
Mehgan Oswald, DMD, MD
Resident
Northwell Mather Hospital
Port Jefferson, New York- GL
George Lasker, MD, PhD
attending psychiatrist
Northwell
Port Jefferson, New York - GL
George Lasker, MD, PhD
attending psychiatrist
Northwell
Port Jefferson, New York - SK
Saad Khan, DO FAPA
Senior Medical Officer
Optum Home Based Medical Care
Woodbury, New York - SK
Saad Khan, DO FAPA
Senior Medical Officer
Optum Home Based Medical Care
Woodbury, New York
Presenting Author(s)
Co-Author(s)
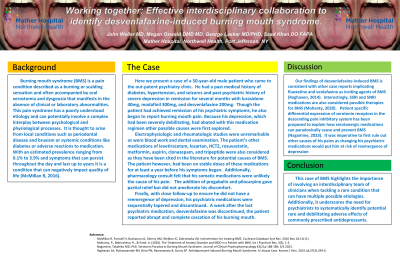
Background:
Burning mouth syndrome (BMS) is a pain condition described as a burning or scalding sensation and often accompanied by oral xerostomia and dysgeusia that manifests in the absence of clinical or laboratory abnormalities. This pain syndrome has a poorly understood etiology and can potentially involve a complex interplay between psychological and physiological processes. It is thought to arise from local conditions such as periodontal disease and bruxism or systemic conditions like diabetes or adverse reactions to medication. With an estimated prevalence ranging from 0.1% to 3.9% and symptoms that can persist throughout the day and last up to years it is a condition that can negatively impact quality of life (McMillan R, 2016).
Case:
Here we present the case of a 50-year-old male in long term psychotherapy who was referred to partial hospitalization (PHP) for worsening depression. Following a lengthy admission to PHP, where he was stabilized on a medication regimen which included desvenlafaxine, he presented to our clinic for ongoing depression management but also complaining of a burning mouth. Given the nature of the complaint, somatic causes were first explored. He was referred for electrophysiologic, rheumatologic lab workup, and dental examination which were unremarkable. Pharmacology consult felt that his somatic medications were unlikely the cause of his pain. Finally, with close follow-up to ensure he did not have a reemergence of depression, his psychiatric medications were sequentially tapered and discontinued. Several days after desvenlafaxine was stopped, he had complete relief of his burning mouth symptoms.
Discussion:
Our findings of desvenlafaxine-induced BMS is consistent with other case reports implicating fluoxetine and venlafaxine as inciting agents of BMS (Raghaven, 2014). Interestingly, SSRI and SNRI medications are also considered possible therapies for BMS (Mohanty, 2020). Patient specific differential expression of serotonin receptors in the descending pain inhibitory system has been proposed to explain how serotonergic medications can paradoxically cause and prevent BMS (Nagamine, 2023). It was imperative to first rule out other causes of his pains as changing his psychiatric medications would put him at risk of reemergence of depression. This case of BMS highlights the importance of involving an interdisciplinary team of clinicians when tackling a rare condition that can have multiple possible etiologies. Additionally, it underscores the need for psychiatrists to systematically identify potential rare and debilitating adverse effects of commonly prescribed antidepressants.
References:
McMillan R, Forssell H, Buchanan JA, Glenny AM, Weldon JC, Zakrzewska JM. Interventions for treating BMS. Cochrane Database Syst Rev. 2016 Nov 18;11(11)
Mohanty, P., Bobrysheva, H., & Patel, A. (2020). The Treatment of Anxiety Disorder and MDD in a Patient with BMS. Int J Psychiatr Res, 3(5), 1-3.
Nagamine, Takahiko MD, PhD. Serotonin Paradox in Burning Mouth Syndrome. Journal of Clinical Psychopharmacology 43(2):p 188-189, 3/4 2023.
Raghavan SA, Puttaswamiah RN, Birur PN, Ramaswamy B, Sunny SP. Antidepressant-induced Burning Mouth Syndrome: A Unique Case. Korean J Pain. 2014 Jul;27(3):294-6.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: Stigma surrounding pain patients can be a significant barrier to proper diagnosis and management. Patients from marginalized or minority communities may face additional layers of stigma due to factors such as race, ethnicity, socioeconomic status, or gender identity. A consult liaison psychiatrist, through their training in psychiatry can address and challenge these stigmas effectively. As psychiatrists we often take a holistic approach to patient care, considering not only the physical symptoms but also the psychological, social, and cultural factors influencing health and well-being.

