Neurocognitive Disorders and Neuropsychiatry
(107) When Visual Impairment Manifests Hallucinations: A Review of Charles Bonnet Syndrome

Thomas Caussat, Bachelor's of Science
MS4
Florida Atlantic University College of Medicine
Boca Raton, Florida
Jake Teich, MD
Psychiatry Resident
FAU College of Medicine
Boca Raton, Florida
Presenting Author(s)
Co-Author(s)
Background/Significance:
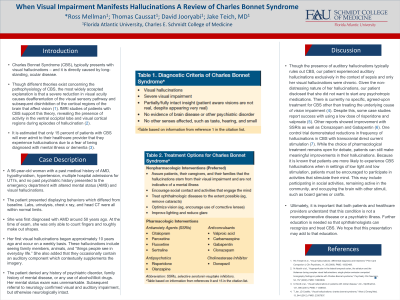
Charles Bonnet Syndrome (CBS) often manifests as visual hallucinations, stemming from long-standing ocular diseases. Predominantly, CBS's pathophysiology is believed to be due to significant visual acuity reduction, leading to deafferentation in the visual sensory pathway and disinhibition in the brain's vision-related cortical areas. This is supported by fMRI studies showing activity in the ventral occipital lobe and visual cortex during hallucinatory episodes (Adachi, 2000). Interestingly, only about 15% of CBS patients report their hallucinations, fearing misdiagnosis of mental illness or dementia (Scott, 2001).
Case:
A 96-year-old woman with a past medical history of AMD, hypothyroidism, and hypertension was admitted for reported acute altered mental status associated with chronic visual hallucinations. At the time of exam, she was only able to count fingers and roughly make out shapes. During our consultation, patient admitted to weekly visual hallucinations for roughly ten years. When discussing the specifics of these visual hallucinations, the patient stated that she often sees family members, animals, and “things people see in everyday life.” Neurology consultants agreed with a diagnosis of CBS. Education was provided and the patient, given the non-distressing nature of her hallucinations, preferred no pharmacological treatment.
Discussion:
There is currently no specific, agreed-upon treatment for CBS other than treating the underlying cause of vision impairment (Jan, 2012). Despite this, some case studies report success with using a low dose of risperidone and valproate (Alamri, 2018). Other reports showed improvement with SSRIs as well as Clonazepam and Gabapentin (Jackson, 2009). While the choice of pharmacological treatment remains open for debate, patients can still make meaningful improvements in their hallucinations. Patients are more likely to experience CBS hallucinations in settings of low light and low stimulation, patients should be encouraged to participate in activities that stimulate their mind, such as individual or group activities that they enjoy.
Ultimately, it is important that both patients and healthcare providers understand that this condition is not a neurodegenerative disease or a psychiatric illness. It is our goal to promote recognition of CBS as to improve outcomes for our patients.
References:
Adachi N, Watanabe T, Matsuda H, Onuma T. Hyperperfusion in the lateral temporal cortex, the striatum and the thalamus during complex visual hallucinations: single photon emission computed tomography findings in patients with Charles Bonnet syndrome. Psychiatry Clin Neurosci. 2000 Apr.
Scott IU et al. Visual hallucinations in patients with retinal disease. Am J Ophthalmol, 131, 590 (2001). PMID: 11336933.
Jan T, Del Castillo J. Visual hallucinations: charles bonnet syndrome. West J Emerg Med. 2012 Dec;13(6):544-7.
Alamri SH. A low dose of risperidone resolved Charles Bonnet syndrome after an unsuccessful trial of quetiapine: a case report. Neuropsychiatr Dis Treat. 2018 Mar 20;14:809-811.
Jackson ML, Ferencz J. Cases: Charles Bonnet syndrome: visual loss and hallucinations. CMAJ. 2009 Aug 4;181(3-4):175-6.
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: Our case addresses Charles Bonnet Syndrome (CBS), which manifests in patients with longstanding visual impairment. It is our goal to promote recognition of CBS as to improve outcomes for our patients.

