Catatonia
(037) What internists and neurologists know and think about catatonia

Japsimran Kaur, MD
Resident
University of Pittsburgh Medical Center
Clarksville, Maryland
Mark A. Oldham, MD, FACLP
Associate Professor
University of Rochester Medical Center
Rochester, New York
Presenting Author(s)
Co-Author(s)
Background: Catatonia may be the presenting manifestation of many medical and neurological conditions. Half of reported catatonia cases in acute care settings have a secondary cause.1 As such, acute care practitioners in internal medicine and neurology will care for patients with catatonia. Moreover, they will often be the first clinician to encounter patients presenting with catatonia. It is imperative that these clinicians be aware of catatonia and its clinical features to ensure reliable recognition and treatment planning. We aimed to conduct the first study to understand what internists and neurologists know and think about catatonia, both to raise catatonia awareness among these practitioners and to inform future educational campaigns.
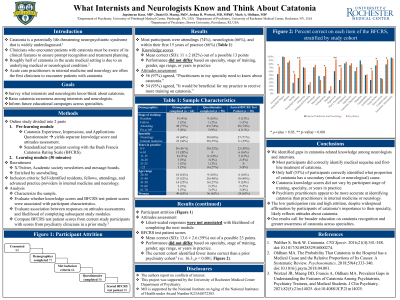
Methods: We conducted an online study disseminated via X/Twitter and academic society newsletters and message boards, enriched by snowballing. Study completers were entered into a raffle for one of three $100 gift cards. Enrollment was open 9/15/23 to 1/15/24. Eligible subjects were attendings, fellows, residents, and advanced-practice providers in internal medicine or neurology. We collected basic demographic/professional information, evaluated catatonia attitudes and knowledge via questionnaire, and catatonia recognition via standardized patient video scoring using the Bush-Francis Catatonia Rating Scale (BFCRS). Finally, subjects were presented with a 30-minute educational module and post-module questionnaires, previously evaluated among psychiatric clinicians.2 Here, we report sample characteristics and describe performance on knowledge-based multiple-choice questions, Likert scale items of attitudes, and BFCRS scoring accuracy. We analyze the association between participant performance and participant characteristics.
Results: Of 99 consented subjects, 75 provided demographics, 64 of whom met inclusion criteria. Fifty-eight (91% of eligible, enrolled subjects) completed the knowledge-based questionnaire, and 38 (59%) scored the BFCRS. Among questionnaire completers, 74% were attendings, 66% were in neurology, and 66% were within their first 15 years of practice. Catatonia knowledge questionnaire scores did not differ based on specialty, stage of training, or years of practice. Whereas 56 (97%) agreed that it is important for practitioners in their specialty to know about catatonia, and 54 (93%) agreed that it would be beneficial for them to receive training on catatonia, these reported attitudes were not associated with the likelihood of completing the next study module of scoring the BFCRS. Mean correct score on BFCRS was 13.6 out of 23 (59%), and accuracy of BFCRS scoring was not associated with stage of training, years of practice, or specialty. Only 16 (25%) completed educational modules.
Discussion: We highlight large gaps in catatonia-related knowledge among internal medicine and neurology practitioners, regardless of specialty, stage of training, or years of practice. We strongly suspect that the low rate of participation and high attrition, despite nearly all subjects’ affirming the importance of catatonia to their specialty and their practice, reflects overall attitudes of catatonia among these specialties. Our results will inform subsequent educational and awareness efforts among internists and neurologists.
1Oldham. The Probability That Catatonia in the Hospital has a Medical Cause and the Relative Proportions of Its Causes. Psychosomatics. DOI:10.1016/j.psym.2018.04.001.
2Wortzel. Evaluating the Effectiveness of an Educational Module for the Bush-Francis Catatonia Rating Scale. Acad Psychiatry. DOI:10.1007/s40596-021-01582-0.
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: The literature suggests that individuals from historically marginalized groups are disproportionately affected by catatonia. A recent case-control study of more than 26,000 patients found that patients with catatonia were more likely to be from ethnic minorities (1). Our study, which identifies gaps in the catatonia-specific knowledge of practitioners in internal medicine and neurology, is an important first step in examining biases among providers when identifying catatonia. Such insight can inform strategies to address these biases, leading to more equitable healthcare practices.
1. Rogers et al. (2023). Catatonia: demographic, clinical and laboratory associations. Psychological medicine, 53(6), 2492–2502.

