Transplant Psychiatry and C-L Subspecialties
(222) Utilizing Mental Health Screenings to Guide Integration of Psychiatric Services within Post-Liver Transplant Clinic

Christopher Parrill, DO
Resident
University of Arkansas for Medical Sciences
Little Rock, Arkansas
Payton Lea, MD
Assistant Professor
University of Arkansas for Medical Sciences
Little Rock, Arkansas- BP
Benjamin P. Pruitt, BS
Medical Student
University of Arkansas for Medical Sciences
Little Rock, Arkansas - MY
Ming Hwei Yek, PsyD
Assistant Professor
University of Arkansas for Medical Sciences
Little Rock, Arkansas
Presenting Author(s)
Co-Author(s)
Background/Significance: Given the increased prevalence of depression in liver transplant (LT) recipients and its impact on transplant outcomes (Annema, 2018), routine screening for depression and referral for a positive screen is recommended for all LT recipients (Zimbrean, 2023). The purpose of this study was to examine the impact of implementing routine mental health screenings for post-LT patients at our small transplant center, and discuss steps to address inconsistent contact with patients after referral.
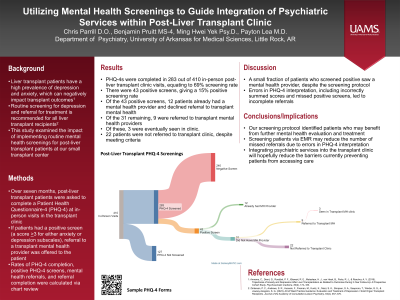
Methods: Over a seven-month period, post-LT patients were asked to complete the Patient Health Questionnaire-4 (PHQ-4) at all in-person visits in the transplant clinic. Following a positive screen (a score >3 for either anxiety or depression subscales), referral to a transplant mental health provider was offered to the patient. Through chart review we calculated the rates of PHQ-4 completion, positive PHQ-4 screens, mental health referrals, and referral completion.
Results: During the seven-month screening period, PHQ-4s were completed in 283 out of 410 in-person post-LT clinic visits, resulting in a 69% completion rate. There were 43 positive screens, giving a 15% positive screening rate. Of these positive screens, only nine out of 31 patients who did not already have a mental health provider were referred to transplant mental health providers, and only three were eventually seen in clinic. Following recognition of the low rate of positive screens successfully being connected with transplant mental health providers, full integration of mental health services in our transplant clinic was begun.
Discussion: ACLP guidelines indicate that patients who screen positive for depression should be referred and evaluated, ideally by a provider with expertise in transplant psychiatry. Our findings indicate that despite implementing screening protocols and identifying patients with mental health needs, only a small fraction of patients who screened positive eventually saw one of our mental health providers. By integrating transplant mental health providers directly in the clinic, we hope to decrease barriers to care access and increase the number of patients successfully completing referral to mental health providers
Conclusion/Implications: While our screening protocol identified patients who could benefit from further mental health evaluation and treatment, the high rate of patients not being seen by mental health providers has led to efforts to integrate mental health providers directly into the transplant clinic. We hope this study will help serve as a guide to other small transplant centers seeking to implement routine mental health screenings post-LT and address low referral completion rates.
References:
Annema, C., Drent, G., Roodbol, P. F., Stewart, R. E., Metselaar, H. J., van Hoek, B., Porte, R. J., & Ranchor, A. V. (2018). Trajectories of Anxiety and Depression After Liver Transplantation as Related to Outcomes During 2-Year Follow-Up: A Prospective Cohort Study. Psychosomatic medicine, 80(2), 174–183.
Zimbrean, P. C., Andrews, S. R., Hussain, F., Fireman, M., Kuntz, K., Niazi, S. K., Simpson, S. A., Soeprono, T., Winder, G. S., & Jowsey-Gregoire, S. G. (2023). ACLP Best Practice Guidance: Evaluation and Treatment of Depression in Solid Organ Transplant Recipients. Journal of the Academy of Consultation-Liaison Psychiatry, 64(4), 357–370.
Presentation Eligibility: The preliminary data for this poster has been accepted as a brief oral abstract at the 2024 American Transplant Congress. This poster being submitted includes an additional four months of data, additional analysis of referrals, and focuses on plans to integrate psychiatric care directly into a post-transplant clinic.
Diversity, Equity, and Inclusion: Our study featured a newly implemented mental health screener in our liver transplant clinic. The inclusion of this screener helps to normalize conversations about mental health among providers, patients, and support staff in clinic. This reduction in stigma can help decrease disparities in patients being connected with mental health care. Additionally, our study focused on filling a gap in provision of mental health care at our transplant clinic, and focused on ways to reduce identified barriers to care access.

