Neurocognitive Disorders and Neuropsychiatry
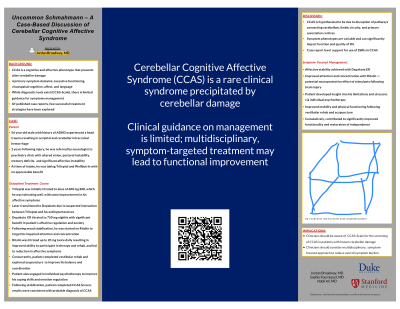
(106) Uncommon Schmahmann – A Case-Based Discussion of Cerebellar Cognitive Affective Syndrome

Jordan Broadway, MD
Fellow
Stanford
Menlo Park, California- SF
Sophie Fourniquet, MD
Resident
Duke Psychiatry
Durham, North Carolina 
Nabil Ali, MD
MD
Central Regional Hospital
HILLSBOROUGH, North Carolina
Presenting Author(s)
Co-Author(s)
Title: Uncommon Schmahmann – A Case-Based Discussion of Cerebellar Cognitive Affective Syndrome Cerebellar Cognitive Affective Syndrome (CCAS) represents a cognitive and affective phenotype following cerebellar damage, demonstrated in four domains: executive dysfunction, visuospatial cognitive deficits, affective instability, and language deficits (Schmahmann, 1988). Diagnosis remained subjective, until Hoche et al. developed a diagnostic scale in 2018 to help standardize diagnostic practices. Though literature describing the syndrome is available, guidance on symptom management is limited (Ahmadian et al, 2019). Of published case reports, few include successful strategies beyond initiation of SSRI (Bhatia et al, 2016). Mr. K is a 58 yo referred to outpatient psychiatry for affective instability, which developed after L occipital intracranial hemorrhage while anticoagulated. He had several hospitalizations, presenting with confusion, visual disturbances, and agitation. MRI demonstrated L occipital lobe and L cerebellar encephalomalacia, and multiple remote L occipital and L cerebellar infarcts. EEG was unremarkable. At presentation, he described postural instability, memory and word retrieval deficits, emotional instability/agitation, and visual hallucinations. He was taking 300 mg Trileptal daily, with mild benefit. Trileptal was titrated, but after blood pressure fluctuations, he was transitioned to Depakote XR, titrated to 750 mg nightly. Ritalin was later added at 20 mg BID to target cognitive symptoms. In addition to psychotropic interventions, his treatment course included vestibular rehabilitation, acupuncture, and cognitive behavioral therapy. His sleep was optimized after a sleep study revealed sleep apnea. Over the following year, he experienced significant improvement in physical, affective, and cognitive ability, with improved functionality. Schmahmann’s syndrome is a clinical condition that develops from cerebellar disease, resulting in both cognitive and affective deficits due to disruption of the reciprocal pathways connecting the cerebellum, limbic circuitry, and primary association cortices. The patient described had features of cerebellar motor syndrome, vestibulo-cerebellar syndrome, and cognitive and affective symptoms consistent with Schmahmann’s syndrome (Manto et, all 2015). Treatment approach was multidisciplinary and symptom-based. Affective stabilization was reached with titration of mood stabilizer. Motor symptoms were addressed with vestibular rehabilitation and acupuncture. Through CBT, patient identified factors that exacerbated symptoms and developed behavioral strategies. Greater symptom reduction was achieved through utilization of a stimulant and optimizing sleep. Collectively, this suggests that a multimodal care plan is beneficial for patients with cerebellar deficits. Clinicians should be aware of psychiatric symptoms with cerebellar disease and should consider a multidisciplinary, multimodal treatment plan to help mitigate cognitive and affective sequala. Ahmadian N, van Baarsen K, van Zandvoort M, Robe PA. The Cerebellar Cognitive Affective Syndrome-a Meta-analysis. Cerebellum. 2019 Oct;18(5):941-950. Bhatia MS, Saha R, Gautam P. Cerebellar Cognitive Affective Syndrome: A Case Report. Prim Care Companion CNS Disord. 2016 Mar 31;18(2) Hoche F, Guell X, Vangel MG, Sherman JC, Schmahmann JD. The cerebellar cognitive affective/Schmahmann syndrome scale. Brain. 2018 Jan 1;141(1):248-270. Manto M, Mariën P. Schmahmann's syndrome - identification of the third cornerstone of clinical ataxiology. Cerebellum Ataxias. 2015 Feb 27;2:2. Schmahmann JD, Sherman JC. The cerebellar cognitive affective syndrome. Brain. 1998 Apr;121 ( Pt 4):561-79. doi: 10.1093/brain/121.4.561. PMID: 9577385.
Background:
Case:
Discussion:
Conclusion:
References:
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: Historically, marginalized groups have not had equal access to psychiatry, and even if available, their mental health concerns have been met with structural, clinical, and diagnostic bias. Using standardized screening tools, such as the screening tool referenced in this submission, helps to eliminate bias and create more uniform and standardized clinical practice. In addition, the co-authors listed for this project represent a rich diversity in personal identity, training, background, clinical interests and career stage.

