Psycho-Oncology and Palliative Care
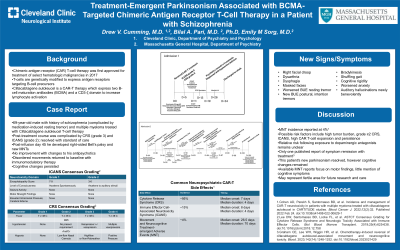
(126) Treatment-Emergent Parkinsonism Associated with BCMA-Targeted Chimeric Antigen Receptor T-Cell Therapy in a Patient with Schizophrenia

Drew Cumming, MD
Physician
Cleveland Clinic
Cleveland, Ohio
Bilal A. Bari, MD, PhD
Resident
Massachusetts General Hospital
Boston, Massachusetts- ES
Emily Sorg, MD
Psychiatrist
Massachusetts General Hospital
Boston, Massachusetts
Presenting Author(s)
Co-Author(s)
Background/Significance: Chimeric antigen receptor (CAR) T-cell therapy was approved for treatment of select hematologic malignancies in 2017 and the clinical indications continue to grow. Currently approved CAR T-cell products target either CD19 or BCMA antigens on tumor cells. While certain side effects of these novel therapies are well-documented, including cytokine release syndrome (CRS) and immune effector cell-associated neurotoxicity syndrome (ICANS), others are less commonly described, including neurotoxicities and movement disorders that may be reversible. To our knowledge there have been no published cases of treatment-emergent parkinsonism in a patient on chronic antipsychotic treatment after receiving CAR T-cell therapy. Case: The patient was a 69 year-old male with a psychiatric history notable for schizophrenia treated with haloperidol decanoate, an unspecified anxiety disorder treated with sertraline, and unspecified insomnia disorder treated with trazodone. He had a mild bilateral hand resting tremor treated with benztropine. He further had a medical history of multiple myeloma, initially treated with daratumumab/velcade/lenalidomide and focal radiation, followed by melphalan and autologous stem cell transplant (ASCT), and ultimately with ciltacabtagene autoleucel BCMA-targeted CART-cell therapy. Following his ASCT, nightly and as-needed olanzapine was added for worsened anxiety in the setting of high-dose steroids. The patient’s post-CART-cell therapy course was complicated by grade 3 CRS and grade 2 ICANS. Forty-five days after treatment, he developed a new right-sided Bell’s palsy with dysarthria, followed by dysphagia, shuffling gait, worsened bilateral rest tremor, new postural and intention tremors, bradykinesia and cogwheel rigidity. His haloperidol was converted to an oral formulation and cross-tapered to monotherapy with olanzapine without significant change in symptoms. He was treated with cyclophosphamide, anakinra and dexamethasone with resolution of rigidity, return to baseline tremor, and improved orofacial symptoms. Discussion: To our knowledge this is the first reported case of treatment-emergent parkinsonism following BCMA-targeted CART-cell therapy in a patient on long-standing antipsychotic treatment. Prior reports of associated parkinsonism have not reported positive response to carbidopa/levodopa and have demonstrated intact dopamine uptake within the basal ganglia on PET-FDG (Gust, 2023). This may suggest a site of action downstream from the postsynaptic D2 receptors which are impacted by antipsychotic medications, however this remains to be determined. Importantly, with immunosuppression, our patient’s parkinsonism largely resolved, adding to the few existing case reports of successful treatment of ciltacabtagene autoleucel-associated movement and neurocognitive toxicity. Conclusion/Implication: This case highlights a potential side effect of a new cancer immunotherapy with phenotypic overlap with that of antipsychotic side effect(s). As consultation-liaison psychiatrists are often consulted to assess possible side effects of psychotropic medications, this case importantly draws attention to the different underlying pathology leading to CART-cell-associated parkinsonism. This will help clinicians at the bedside avoid unnecessary medication changes and guide the treatment approach accordingly. References Gust J. (2023). BCMA-CAR T-cell treatment-associated parkinsonism. Blood, 142(14), 1181–1183. https://doi.org/10.1182/blood.2023021860
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: This case reports on a rarely described side effect (parkinsonism) of a growing oncologic therapy. This side effect can mirror that seen in patients receiving antipsychotics, putting a vulnerable population at risk of unnecessary medication changes and potential destabilization.
The authors include two trainees.

