Catatonia
(033) The Many Faces of Gabapentin Withdrawal

Rijah Chhapra, MD (she/her/hers)
Resident
University of Kentucky
Lexington, Kentucky
Lynda Eckhardt, PharmD, MBA, BCPS, AAHIVP
Adult Inpatient Psychiatry and Internal Medicine Clinical Pharmacist
University of Kentucky HealthCare
Lexington, Kentucky- SO
Sarah Oros, MD
Assistant Professor
Psychiatry
Lexington, Kentucky
Presenting Author(s)
Co-Author(s)
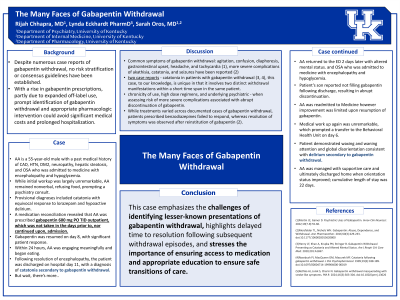
Background: Despite numerous case reports of gabapentin withdrawal, no risk stratification or consensus guidelines have been established. With a rise in gabapentin prescriptions, partly due to expanded off-label use, prompt identification of gabapentin withdrawal and appropriate pharmacologic intervention could avoid significant medical costs and prolonged hospitalization.
Case: AA is a 55-year-old male with a past medical history of CAD, HTN, DM2, neuropathy, hepatic steatosis, and OSA who was admitted to Medicine with encephalopathy and hypoglycemia. While initial workup was largely unremarkable, AA remained nonverbal, refusing food, prompting a Psychiatry consult. Provisional diagnoses included catatonia with equivocal response to lorazepam and hypoactive delirium. A medication reconciliation revealed that AA was prescribed gabapentin 600 mg PO TID outpatient, which was not taken in the days prior to, nor continued upon, admission. Gabapentin was resumed on day 8, with significant patient response. Within 24 hours, AA was engaging meaningfully and began eating. Following resolution of encephalopathy, the patient was discharged on hospital day 11, with a diagnosis of catatonia secondary to gabapentin withdrawal. AA returned to the ED 2 days later with altered mental status. Patient’s son reported not filling gabapentin following discharge, resulting in abrupt discontinuation. AA was readmitted to Medicine however improvement was limited upon resumption of gabapentin. Medical work up again was unremarkable, which prompted a transfer to the Behavioral Health Unit on day 6. Patient demonstrated waxing and waning attention and global disorientation consistent with delirium secondary to gabapentin withdrawal. AA was managed with supportive care and ultimately discharged home when orientation status improved; cumulative length of stay was 22 days.
Discussion:
Gabapentin withdrawal has been most often characterized by symptoms of agitation, confusion, diaphoresis, gastrointestinal upset, headache, and tachycardia (Martin, 2022), however more severe complications of akathisia, catatonia, and seizures have been reported (Mersfelder, 2016). While two case reports have described catatonia in patients with gabapentin withdrawal (Henry, 2020; Rosebush, 1999), this case, to our knowledge, is unique in that it involves two distinct withdrawal manifestations within a short time span in the same patient. Factors such as chronicity of use, high dose regimens, and underlying psychiatric conditions should be evaluated when assessing risk of more severe complications associated with abrupt discontinuation of gabapentin. While treatments varied across documented cases of gabapentin withdrawal, patients prescribed benzodiazepines failed to respond, whereas resolution of symptoms was observed after reinstitution of gabapentin (Mersfelder, 2016). Martin JC, Gainer D. Psychiatric Uses of Gabapentin. Innov Clin Neurosci. 2022;19(7-9):55-60. Mersfelder TL, Nichols WH. Gabapentin: Abuse, Dependence, and Withdrawal. Ann Pharmacother. 2016;50(3):229-233. doi:10.1177/1060028015620800 Rosebush PI, MacQueen GM, Mazurek MF. Catatonia following gabapentin withdrawal. J Clin Psychopharmacol. 1999;19(2):188-189. doi:10.1097/00004714-199904000-0001
Conclusion: This case emphasizes the challenges of identifying lesser-known presentations of gabapentin withdrawal, highlights delayed time to resolution following subsequent withdrawal episodes, and stresses the importance of ensuring access to medication and appropriate education to ensure safe transitions of care.
References:
Henry LF, Khan A, Krupka PN, Stringer B. Gabapentin Withdrawal Presenting as Catatonia and Altered Mental Status. Am J Respir Crit Care Med. 2020;201:A1697.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: This case sheds light on an often overlooked aspect of healthcare, particularly in the context of withdrawal. Historically marginalized groups, such as low-income individuals or those with limited access to healthcare, may face additional barriers when dealing with medication withdrawal due to lack of resources, access or knowledge, which could inadvertently lead to delayed time to resolution and potentially exacerbating health disparities.

