Cardiology
(010) Is It Really Ever A Pheo? Understanding Paroxysmal Hypertension

Samantha DeSilva, MD
Psychiatry Resident PGY3
AtlantiCare Regional Medical Center
Atlantic City, New Jersey- KS
Keith Semler, DO
Chief Resident
AtlantiCare Regional Medical Center
Egg Harbor Township, New Jersey - RD
Roshi DeSilva, DO
Consult Liaison Psychiatrist
AtlantiCare Regional Medical Center
Pomona, New Jersey
Presenting Author(s)
Co-Author(s)
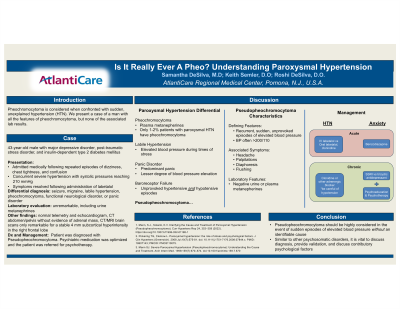
Background/Significance: Pheochromocytoma is always considered when confronted with sudden, unexplained hypertension. When this diagnosis is ruled out, the condition is often left undiagnosed and untreated leading to the potential for significant impairment and disability (Mann, 1999). 1 Mann, S.J., Solanki, K.V. Clarifying the Cause and Treatment of Paroxysmal Hypertension (Pseudopheochromocytoma). Curr Hypertens Rep 24, 353–359 (2022). https://doi.org/10.1007/s11906-022-01198-1 2 Pickering TG, Clemow L. Paroxysmal hypertension: the role of stress and psychological factors. J Clin Hypertens (Greenwich). 2008 Jul;10(7):575-81. doi: 10.1111/j.1751-7176.2008.07844.x. PMID: 18607143; PMCID: PMC8110075. 3 Mann SJ. Severe Paroxysmal Hypertension (Pseudopheochromocytoma): Understanding the Cause and Treatment. Arch Intern Med. 1999;159(7):670–674. doi:10.1001/archinte.159.7.670
Case: A 43-year-old male with major depressive disorder, post-traumatic stress disorder, and insulin-dependent type 2 diabetes mellitus was admitted medically following repeated episodes of dizziness, chest tightness, and confusion. Subsequent episodes while hospitalized revealed concurrent severe hypertension with systolic pressures reaching 210 mmHg. Symptoms resolved following administration of labetalol. Initial differential diagnosis included seizure, migraine, labile hypertension, pheochromocytoma, functional neurological disorder, or panic disorder. Laboratory evaluation, including urine metanephrines, was unremarkable. Other findings included telemetry without signs of arrhythmia, normal echocardiogram, CT abdomen/pelvis without evidence of adrenal mass, and CT/MRI brain scans only remarkable for a stable 4 mm subcortical hyperintensity in the right frontal lobe. Given these results, paroxysmal hypertension was deemed the most accurate diagnosis. Psychiatric medication was optimized and the patient was referred for psychotherapy.
Discussion: Paroxysmal hypertension, or pseudopheochromocytoma, is characterized by recurrent, sudden, unprovoked episodes of elevated blood pressure with associated symptoms of headache, palpitations, diaphoresis, and flushing. Paroxysmal hypertension may easily be mistaken for a panic attack given the sudden, unexpected nature and lack of other readily identifiable causes. However, Mann et. al argue that distinguishing features of paroxysmal hypertension include marked blood pressure elevation and absence of emotional distress. Pickering & Clemow suggest that both conditions may represent different facets of the same underlying syndrome. Regardless, most literature agrees that key features of treatment should include acute management of paroxysms with clonidine and/or an anxiolytic agent, discussion with patient of psychological origin, and psychopharmacologic management (Mann, 2022; Pickering & Clemow, 2008). SSRIs or tricyclic antidepressants at therapeutic doses have shown efficacy in successfully mitigating the frequency of attacks. Adrenergic blockade may be indicated in some cases, but must be used cautiously with normal or low baseline blood pressures (Mann, 1999). Psychological intervention is a critical component of treatment as these patients commonly suffer from an underlying history of trauma that may or may not be repressed (Mann, 2022).
Conclusions: Paroxysmal hypertension should be highly considered in the event of sudden episodes of elevated blood pressure without an identifiable cause. Diagnosis is complicated by lack of objective data. Similar to other psychosomatic disorders, it is vital to provide validation and discuss contributory psychological factors.
References:
Presentation Eligibility: N/A
Diversity, Equity, and Inclusion: Minority groups in the United States, specifically Black Americans, are disproportionately affected by both hypertension and trauma disorders. Additionally, minority groups are dismissed as non-adherent to treatment plans, when really there is an undiagnosed underlying pathology. Better understanding paroxysmal hypertension will allow healthcare providers to equitably treat our patients of diverse backgrounds.

