Diversity, Equity, and Inclusion
(073) Integration of Trans-affirming Care Across General Hospital Settings

Antoine Beayno, MD
Psychiatry Resident
Mount Sinai Health System
NEW YORK, New York- YA
Yekaterina Angelova, MD
Director of Consultation-Liaison Psychiatry
NYC H+H Harlem
NEW YORK, New York
Presenting Author(s)
Co-Author(s)
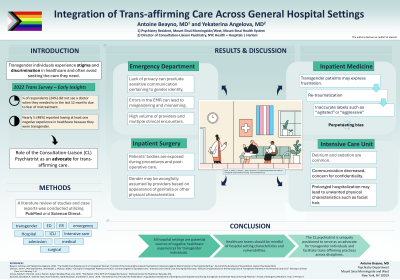
Background: Transgender individuals experience significant stigma and healthcare disparities, often resulting in avoidance of healthcare settings (James, 2016). The consultation-liaison psychiatrist can occupy an invaluable role in advocacy and integration of trans-affirming care in a variety of hospital settings. Methods: A literature review of studies and case reports was conducted utilizing PubMed and Science Direct. Search terms included “transgender” and one of the following: “ED,” “ER,” “emergency,” “hospital,” “ICU, “intensive care,” “hospital,” “admission, “medical,” and “surgical.” We focused on potential sources of disparity and distress for transgender individuals admitted to various hospital settings. Results/Discussion: Transgender individuals face significant challenges in emergency rooms (ED), surgical wards, medical wards and intensive care units (ICU). In the ED, lack of privacy often precludes sensitive communication pertaining to gender identity. Errors in the electronic medical record may predispose to misgendering and deadnaming, especially given multiple brief encounters with a high volume of providers in the ED (Samuels, 2018). Transgender patients in the hospital setting may express frustration with negative healthcare experiences and re-traumatization and be inaccurately labeled as “aggressive” or “agitated,” further perpetuating bias (Beayno, 2022). Surgical settings, where patient’s bodies are exposed during procedures and post-operative care, are especially prone to non-affirming care as gender may be wrongfully assumed by providers based on appearance of genitalia or other physical characteristics. In the ICU, where sedation and delirium are common, transgender patients may not be able to communicate their correct name, gender identity and pronouns. Providers must balance the benefits of collateral from family and proxies against the risk of disrespecting patients’ confidentiality or “outing” them. Prolonged hospitalizations may lead to development of unwanted physical characteristics such as facial hair; care teams should be mindful of attending to patients’ hygiene and grooming, and consider other ways to ensure comfort and satisfaction (Gilmore, 2024). Conclusion: All general hospital settings are potential sources of negative healthcare experiences, re-traumatization and disparity for transgender individuals. The consultation-liaison psychiatrist is uniquely positioned to serve as an advocate for transgender individuals across hospital settings and facilitate trans-affirming practices across disciplines. References: Beayno, Antoine, and Yekaterina Angelova. 2022. “The Health Care Experience of a Transgender Woman: The Role of the Consultation-Liaison Psychiatrist in Advocacy Against Discrimination in the Hospital Setting.” Journal of the Academy of Consultation-Liaison Psychiatry 63 (4): 400–403. https://doi.org/10.1016/j.jaclp.2021.10.001. Gilmore, John P., Marissa Dainton, and Natalie L. McEvoy. 2024a. “Caring for Transgender Patients in the ICU: Current Insights for Equitable Care.” Intensive and Critical Care Nursing 82 (February): 103657. https://doi.org/10.1016/j.iccn.2024.103657. James, Sandy E.; Herman, Jody L; Rankin, Susan; Keisling, Mara et al. 2016. “The Report of the 2015 US Transgender Survey.” National Center for Healthcare Equality, 302. Samuels, Elizabeth A., Chantal Tape, Naomi Garber, Sarah Bowman, and Esther K. Choo. 2018. “‘Sometimes You Feel Like the Freak Show’: A Qualitative Assessment of Emergency Care Experiences Among Transgender and Gender-Nonconforming Patients.” Annals of Emergency Medicine 71 (2): 170-182.e1. https://doi.org/10.1016/j.annemergmed.2017.05.002.
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: The topic presented highlights important healthcare disparities experienced by the transgender community. Transgender individuals are at increased risk of stigma and discrimination and that includes healthcare settings. Studies have shown that the experiences of misgendering or deadnaming can lead to psychological distress, and subsequently lead to reluctance to seek health care needed. We highlight ways that the Consultation-Liaison Psychiatrist can advance trans-affirming care in the general hospital setting, thus improving mental health outcomes for this marginalized population.

