Transplant Psychiatry and C-L Subspecialties
(214) Integrating Psychiatry and Psychology within a Heart Transplant Program: Logistics, Benefits, and Challenges

Jesse Allen-Dicker, PhD
Assistant Professor of Psychology in Clinical Psychiatry
Weill Cornell Medicine/NewYork-Presbyterian
New York, New York
Jesse Allen-Dicker, PhD
Assistant Professor of Psychology in Clinical Psychiatry
Weill Cornell Medicine/NewYork-Presbyterian
New York, New York
Karanbir Padda, MD
Assistant Professor of Clinical Psychiatry
New York-Presbyterian | Weill Cornell Medicine
New York, New York
Karanbir Padda, MD
Assistant Professor of Clinical Psychiatry
New York-Presbyterian | Weill Cornell Medicine
New York, New York
Presenting Author(s)
Co-Author(s)
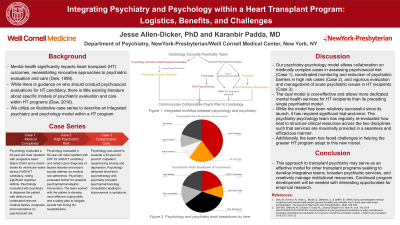
Cases: Our HT center established a model of a 0.4 full-time equivalent (FTE) psychologist and 0.1 FTE psychiatrist working collaboratively to provide psychiatric evaluation and care for HT candidates. We present three cases to illustrate clinical approach in this model: 1) Psychology evaluated a 64-year-old male inpatient with congestive heart failure (CHF) and a recent stroke for ventricular assist device (VAD)/HT candidacy, noting significant cognitive deficits. Psychology consulted with psychiatry to diagnose the patient with delirium and understand relevant medical factors, prognosis, and implications on psychosocial risk. 2) Psychology evaluated a 60-year-old male inpatient with CHF for VAD/HT candidacy and noted a prior diagnosis of bipolar disorder and recent suicide attempt via medical non-adherence. Psychiatry evaluated further for potential psychopharmacological intervention. The team worked with the patient to develop more effective coping skills and a safety plan to mitigate suicide risk during his hospitalization. 3) Psychology was asked to evaluate a 52-year-old post-HT outpatient experiencing anxiety and depression. Psychology delivered short-term psychotherapy and psychiatry provided psychopharmacology consultation leading to improvement in symptoms. Dew, M., Kormos, R., Roth, L., Murali, S., DiMartini, A., & Griffith, B. (1999). Early post-transplant medical compliance and mental health predict physical morbidity and mortality one to three years after heart transplantation. The Journal of Heart and Lung Transplantation, 18(6), 549–562. Dew MA, DiMartini AF, Dobbels F, Grady KL, Jowsey-Gregoire SG, Kaan A, et al. The 2018 ISHLT/APM/AST/ICCAC/STSW recommendations for the psychosocial evaluation of adult cardio- thoracic transplant candidates and candidates for long-term mechanical circulatory support. J Heart Lung Transplant. 2018;37(7): 803–23.
Background: Mental health significantly impacts heart transplant (HT) outcomes, necessitating innovative approaches to psychiatric evaluation and care (Dew, 1999). While there is guidance on who should conduct psychosocial evaluations for HT candidacy, there is little existing literature about specific models of psychiatric evaluation and care within HT programs (Dew, 2018). Here, we utilize an illustrative case series to describe an integrated psychiatry and psychology model within a HT program.
Discussion: Our psychiatry-psychology model allows collaboration on medically complex cases in assessing psychosocial risk (Case 1), vigorous evaluation and management of acute psychiatric issues in HT recipients (Case 2), and coordinated monitoring and reduction of psychiatric barriers in high risk cases (Case 3). The dual model is cost-effective and allows more dedicated mental health services to HT recipients than its preceding single psychiatrist model. While the model has been relatively successful since its launch, it has required significant trial-and-error. The psychiatry-psychology team has regularly re-evaluated how best to structure clinical resources across the two disciplines such that services are maximally provided in a seamless and efficacious manner. Additionally, the team has faced challenges in helping the greater HT program adapt to this new model.
Conclusion: This approach to transplant psychiatry may serve as an effective model to other transplant programs seeking to develop integrative teams, broaden psychiatric services, and creatively manage institutional resources. Continued program development will be needed with interesting opportunities for empirical research.
References:
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: Our submission could advance diversity, equity, and inclusion through its advocacy for greater psychiatric services to be offered to transplant candidates and recipients. Individuals of color and lower socio-economic status have been found to have poorer heart transplant outcomes. Stronger psychiatric services within transplant programs may help further mitigate risk, improve candidacy, and improve outcomes for diverse populations.

