Collaborative and Integrated Care
(058) Improving Health Screening in the General Hospital: A Case Report of a Near-miss Cancer Diagnosis in a Geriatric Patient with Psychosis

Norman R. Greenberg, MD (he/him/his)
Resident Physician
Weill Cornell Medical Center, Department of Psychiatry
New York City, New York
Heather Kawalick, MD
Geriatric Psychiatrist
NYS OMH
NEW YORK, New York
Presenting Author(s)
Co-Author(s)
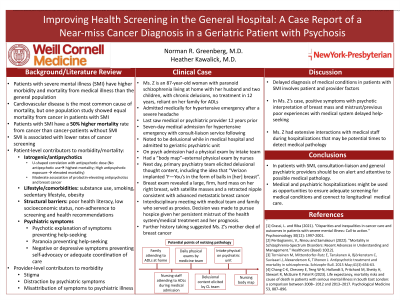
Background
Several factors contribute to the elevated mortality of patients with schizophrenia from medical causes (Peritogiannis, 2022). Stigma and distraction of providers by seemingly more pressing concerns like patients’ psychiatric symptoms, contribute to suboptimal medical care (Aggarwal, 2013; Peritogiannis, 2022). Patients with psychotic illness have higher mortality from cancer, specifically, often due to delayed diagnosis (Grassi, 2021; Peritogiannis, 2022). Herein, we report the case of a patient with schizophrenia who traversed multiple medical settings before providers identified a malignant breast mass.
Case
Ms. Z is an 87-year-old woman with long-standing schizophrenia who last saw a medical or psychiatric provider twelve years ago. She was admitted medically for hypertensive emergency after being brought to the emergency room for a severe headache. Prior to this, she had been living at home dependent on her family, with chronic delusions. During her seven-day medical admission for hypertensive emergency, she was noted to be psychotic by the consult-liaison psychiatry team, was medically cleared, and then admitted psychiatrically. Upon psychiatric admission, Ms. Z was physically examined by the intake medical team. Shortly afterwards, on comprehensive evaluation, the primary psychiatry team elicited among Ms. Z’s persecutory delusions the idea that “Verizon implanted ‘F—Yous’ in the form of small balls in [her] breast”. Concerned that there was a connection between an underlying breast abnormality and her delusions, a breast exam was performed, revealing a large, firm, hard mass on her right breast, with satellite masses and a retracted nipple. Subsequent chart review and history revealed that the abnormal breast findings were not noticed by family members who attended to Ms. Z’s ADLs, or documented during medical admission or initial physical exam on psychiatric admission. Further history-taking revealed that Ms. Z’s mother died of breast cancer.
Discussion
Ms. Z’s case highlights factors that contribute to delayed diagnosis in psychotic patients, including the psychotic interpretation of her breast masses and a decade without medical care. During medical admissions, consult-liaison psychiatrists can help facilitate improvement in medical care for psychotic patients by advocating for more comprehensive physical exams and medical care that is generally reserved for primary care settings. Next, when eliciting delusional thought content from psychotic patients, careful attention to somatic content can be a useful clue to possible medical pathology. Lastly, further education of nurses who have direct roles in attending to patients’ ADLs on medical and psychiatric units, could help with detecting medical abnormalities.
Conclusion
Psychiatrists may utilize medical and psychiatric hospitalizations as opportunities to lower mortality in psychotic patients, by advocating for more comprehensive medical screening and attending to delusional somatic content.
References
Aggarwal, A., Pandurangi, and Smith (2013). "Disparities in breast and cervical cancer screening in women with mental illness: a systematic literature review." Am J Prev Med 44(4): 392-398.
Grassi, L. and Riba (2021). "Disparities and inequalities in cancer care and outcomes in patients with severe mental illness: Call to action." Psychooncology 30(12): 1997-2001.
Peritogiannis, V., Ninou and Samakouri (2022). "Mortality in Schizophrenia-Spectrum Disorders: Recent Advances in Understanding and Management." Healthcare (Basel) 10(12).
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: Inequities in medical care exist for psychotic patients. This poster advocates for more comprehensive medical care for this population.

