Systems-Based Practice, Leadership, and Administrative Psychiatry
(191) Improving “cancel culture:” Implementing a structured process for cancelling inpatient psychiatry consultations while targeting preservation of care quality and augmentation of trainee competency

Bennis Pavisian, D.O. (he/him/his)
Resident Physician
The Ohio State University
Columbus, Ohio- SC
Sana Chughtai, MD
Resident Physician
The Ohio State University Wexner Medical Center
Columbus, Ohio 
Mounika P. Ganguly, MD
Consultation-Liaison Psychiatrist
Nationwide Children's Hospital
Columbus, Ohio
Shazadie Soka, MD
Assistant Professor, Clinical
Wayne State University
Detroit, Michigan- LT
Laura Taylor, DO
Assistant Clinical Professor
The Ohio State University
Columbus, Ohio 
Anita Chang, DO
Clinical Assistant Professor of Psychiatry
Ohio State University
Columbus, Ohio- JN
Joshua L. Norman, DO, FACLP
Psychiatrist
The Ohio State University
Columbus, Ohio 
Kevin Johns, MD
Assistant Clinical Professor
The Ohio State University
Hilliard, Ohio
David Kasick, MD, DFAPA, FACLP
Professor of Clinical Psychiatry and Behavioral Health
The Ohio State University Wexner Medical Center
Columbus, Ohio
Presenting Author(s)
Co-Author(s)
Background: As inpatient hospital care becomes increasingly complex, the growing demand for inpatient psychiatric consultations requires preservation of operational efficiency, medical triage skills, and consultation threshold management. Among current response models, limited attention has been given to consultation order cancellations when clinical problems can be safely addressed through provider education or outpatient referrals (Grover, 2023). To preserve continued care quality, inter-professional teaming, and optimize use of resources, we developed and implemented a structured process on our academic medical center’s inpatient psychiatry consultation-liaison service to teach and analyze the impact of cancelled consultation orders.
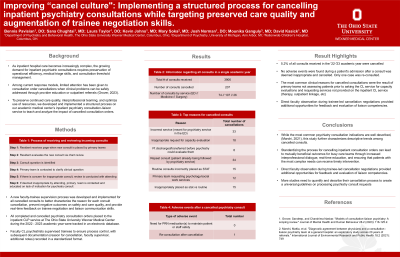
Methods: A new faculty-trainee supervision process was developed and implemented for all cancelled consults to better characterize the reason for each consult cancellation, prevent negative outcomes on safety and care quality, and provide real-time feedback on trainee negotiation and liaison communication skills. All completed and cancelled psychiatry consultation orders placed to the inpatient CLP service at The Ohio State University Wexner Medical Center during the 2023 academic year were tracked in an electronic database. Faculty CL psychiatrists supervised trainees to ensure process control, with subsequent documentation (reason for cancellation, faculty supervisor, additional notes) recorded in a standardized format.
Results: 3906 new psychiatry consultation orders were placed between 7/1/2022 and 6/30/2023. Of these, 207 were cancelled. Retrospective chart review assessed the impact of the cancellation process and indicators of negative outcomes or treatment delays (adverse events, need for emergency medications, re-consultation, or engagement of different specialty team). The most common reason for cancellation was incorrect order (meant for the ED psychiatry team, a separate service), requests surrounding decision-making capacity resolved through provider education, and requests for outpatient-based services that are outside the scope of the inpatient environment. Additional patient-level outcomes are still under investigation.
Discussion: While the most common psychiatry consultation indications are well described, (Marchi, 2021), this study further characterizes descriptive trends among cancelled consults. While our process was initially focused on ensuring efficient use of team resources without compromising patient safety and care quality, we also identified gaps in provider knowledge and system resource needs from the pattern of cancelled consults that were used to create targeted provider education and system requests for funding additional services. Direct faculty observation during trainee-led cancellation negotiations provided additional opportunities for feedback and evaluation of liaison competencies.
Conclusion: Standardizing the process for cancelling inpatient consultation orders can lead to mutually beneficial outcomes for busy care teams through increased inter-professional dialogue, real-time education, and ensuring that patients with the most complex needs can receive timely intervention. For trainees, negotiating service engagement is an interpersonal communication and systems-based practice competency that can benefit from direct faculty supervision.
References:
< ! Grover, Sandeep, and Chandrima Naskar. "Models of consultation-liaison psychiatry: A scoping review." Journal of Mental Health and Human Behaviour 28.2 (2023): 116-125.2.
Marchi, Mattia, et al. "Diagnostic agreement between physicians and a consultation–liaison psychiatry team at a general hospital: an exploratory study across 20 years of referrals." International Journal of Environmental Research and Public Health 18.2 (2021): 749.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: Our project describes an innovative quality improvement process that ensures continual access to inpatient consultation resources for our most vulnerable patients. In addition to optimizing service alignment with levels of integrative complexity that fluctuate during inpatient hospital care, we also aimed to improve resident negotiation skills, promote provider awareness of a range of behavioral health services available across our health system, and preserve safe outcomes when immediate bedside interventions were deferred to an alternate intervention.

