Transplant Psychiatry and C-L Subspecialties
(213) Impact of Second-Generation Antipsychotic Use in Pediatric Bone Marrow Transplant Engraftment: A Case Series.
- IP
Ivan E. Pagan Colon, MD
Consultation-Liaison Fellow
National Institutes of Health / Georgetown School of Medicine
Washington DC, District of Columbia - IP
Ivan E. Pagan Colon, MD
Consultation-Liaison Fellow
National Institutes of Health / Georgetown School of Medicine
Washington DC, District of Columbia - HR
Haniya Raza, DO, FACLP
Chief, Psychiatry Consultation-Liaison Service
National Institute of Mental Health
Bethesda, Maryland - HR
Haniya Raza, DO, FACLP
Chief, Psychiatry Consultation-Liaison Service
National Institute of Mental Health
Bethesda, Maryland 
Michael Liu, B.S.
Research Assistant
National Institute of Mental Health
Rolling Hills Estates, California
Michael Liu, B.S.
Research Assistant
National Institute of Mental Health
Rolling Hills Estates, California.jpg)
Maryland Pao, MD
Clinical & Deputy Scientific Director
National Institutes of Health
Bethesda, Maryland.jpg)
Maryland Pao, MD
Clinical & Deputy Scientific Director
National Institutes of Health
Bethesda, Maryland
Presenting Author(s)
Co-Author(s)
Background
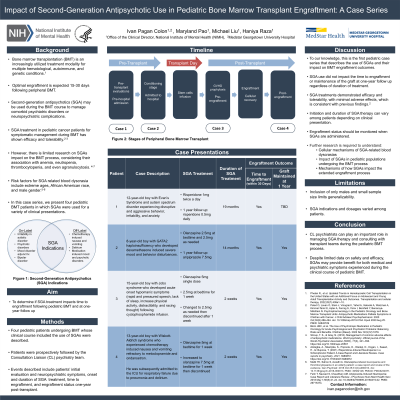
Pediatric bone marrow transplantation (BMT) is an increasingly utilized treatment modality for multiple hematological, autoimmune, and genetic conditions (Phelan, 2022). BMT involves a conditioning regimen, administering hematopoietic stem cells to patients with a depleted bone marrow, and post-transplant surveillance. Engraftment is expected 15-30 days following transplant.
A complex process, BMT may be associated with a variety of psychiatric sequelae, including depression, anxiety, irritability, and delirium leading to use of psychotropic medications during transplant (Nakamura, 2019). Children and adolescents with previously diagnosed neurodevelopmental or mental health disorders, may be at increased risk of developing psychiatric adverse events during cancer therapy and BMT. Second-generation antipsychotics (SGA) have shown benefit in managing symptoms, including irritability, loss of appetite, sleep problems and nausea (Peled, 2020). SGAs may be associated with several adverse effects, including blood dyscrasias (Blom, 2022). Given this possible side effect there is limited data on SGA impact on pediatric BMT engraftment. This case series aims to characterize time to engraftment and additional outcomes of four pediatric patients treated with SGA during BMT.
Methods
Four pediatric patients receiving BMT and experiencing neuropsychiatric symptoms treated with SGAs were described. Patients’ treatment course, onset of neuropsychiatric symptoms, SGA response, adverse effects and time to engraftment were assessed from the time of psychiatric consultation until the post-transplant period.
Results
All patients were males, ages 8 to 15 years. All patients engrafted within the expected time frame. Each patient will be described in detail including relevant histories, transplant course, details of psychiatric consultation and treatment course with SGA including adverse effects. Time to engraftment and details of extended follow up after BMT will be presented.
Discussion
Neuropsychiatric symptoms experienced by pediatric patients undergoing BMT may contribute to additional morbidity, treatment delays, and prolonged hospitalization. Prompt treatment, often necessitating SGAs, is important in mitigating these risks. Given potential hematological adverse effects of SGAs, close clinical monitoring for symptoms of anemia, thrombocytopenia, leucopenia, or any other combination should be done to ensure proper function of the bone marrow. Further, specific planning on SGA discontinuation is an important aspect of treatment.
Conclusion
Despite limited data on safety and efficacy, SGA can have benefit for both medical and psychiatric symptoms experienced during the clinical course of pediatric BMT. Further research is needed to understand the mechanisms of how and to what extent these medications impact the pre-engraftment, early and late post-engraftment periods.
References
Phelan R., et al. Updated Trends in Hematopoietic Cell Transplantation in the United States with an Additional Focus on Adolescent and Young Adult Transplantation Activity and Outcomes. Transplantation and cellular therapy, 2022;28(7):409e1–10.
Nakamura Z., et al. Psychiatric Care in Hematopoietic Stem Cell Transplantation, Psychosomatics, 2019; 60(3):227-237.
Peled O, et al. Psychopharmacology in the Pediatric Oncology and Bone Marrow Transplant Units: Antipsychotic Medications Palliate Symptoms in Children with Cancer. J Child Adolescent Psychopharmacology. 2020 Oct;30(8):486-494.
Blom JMC, et al. The Use of Psychotropic Medication in Pediatric Oncology for Acute Psychological and Psychiatric Problems: Balancing Risks and Benefits. Children (Basel). 2022 Nov 30;9(12):1878.
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: In this case series we included patients: pediatric patients, patient from the latinx community, and patient with autism spectrum disorder. This way we are wanted to highlight bone marrow transplant as a procedure that should be accessible to all who patients who requires it regardless of age, ethnicity or mental health conditions under supervised and safe conditions. It also highlights the importance of Consultation-Liaison physicians working with the pediatric population as well as the importance of liaison work with other specialties such as pediatrics.

