Neurocognitive Disorders and Neuropsychiatry
(092) Hypothalamic Demyelination Process Complicated by Functional Neurological Disorder and Regressive Behavior

Andrin Sadikaj, MD
CL Psychiatry Fellow
Icahn School of Medicine at Mount Sinai
New York, New York- PJ
Pricila Jimenez, MD
trainee
New York
New York, New York 
Carrie L. Ernst, MD, FACLP
Associate Professor
Icahn School of Medicine at Mount Sinai
New Rochelle, New York
Presenting Author(s)
Co-Author(s)
Introduction
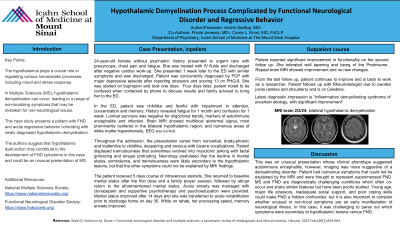
The hypothalamus plays an important role in regulating many homeostatic processes and has been implicated in mood disorders and stress response but is often overlooked when considering the presentation of neuropsychiatric symptoms in conditions such as Multiple Sclerosis (MS). Given the non-localizing nature of many hypothalamic symptoms, there exists a risk of dismissing symptoms as non-neurological. We describe a case of Functional Neurologic Disorder (FND) with acute regressive behavior in the context of newly diagnosed hypothalamic demyelination.
Case Presentation
24-year-old female without psychiatric history presented to urgent care with presyncope, chest pain and fatigue. She was treated with IV fluids and discharged after negative cardiac work-up. She presented 1 week later to the ED with similar symptoms and was discharged. Patient was concurrently diagnosed by PCP with major depressive episode after reporting stressors and scoring 13 on PHQ-9. She was started on bupropion and took one dose. Four days later, patient noted to be confused when contacted by phone to discuss results and family advised to bring her to the ED.
In the ED, patient was childlike and fearful with impairment in attention, concentration and memory. History revealed fatigue for 1 month and confusion for 1 week. Lumbar puncture was negative for oligocloncal bands, markers of autoimmune encephalitis and infection. Brain MRI showed multifocal abnormal signal, most prominently centered in the bilateral hypothalamic region, and numerous areas of white matter hyperintensity. EEG was normal.
Throughout the admission, the presentation varied from nonverbal, bradyphrenic and inattentive to childlike, despairing and anxious with bizarre vocalizations. Patient displayed tremulousness that sometimes evolved into myoclonic jerking with facial grimacing and tongue protruding. Neurology postulated that the decline in mental status, somnolence, and tremulousness were likely secondary to the hypothalamic lesions, but that the other symptoms could not be explained by MRI findings.
The patient received a 5-day course of intravenous steroids. She returned to baseline mental status after the first dose and a family prayer session, followed by abrupt return to the aforementioned mental status. Acute anxiety was managed with clonazepam and supportive psychotherapy and psychoeducation were provided. Mental status improved after 14 days, and she was transferred to acute rehabilitation prior to discharge home on day 35. While on rehab, her processing speed, memory anxiety improved.
Discussion:
This was an unusual presentation whose clinical phenotype suggested autoimmune encephalitis, however imaging was more suggestive of a demyelinating disorder. Patient had numerous symptoms that could not be explained by the MRI and were thought to represent superimposed FND. MS and FND are diagnostically challenging conditions which often co-occur and share similar features but have been poorly studied. Young age, major life stressors, inadequate social support, and poor coping skills could make FND a hidden confounder, but it is also important to consider whether unusual or non-focal symptoms are an early manifestation of neurological illness. In this case, it was challenging to parse out which symptoms were secondary to hypothalamic lesions versus FND.
Presentation Eligibility: "Not previously published or presented"
Diversity, Equity, and Inclusion: MS and FND are diagnostically challenging conditions which often co-occur and share similar features, but have been poorly studied. Young age, major life stressors, inadequate social support, and poor coping skills could make FND a hidden confounder, but it is also important to consider whether unusual or non-focal symptoms are an early manifestation of neurological illness. In this case, it was challenging to parse out which symptoms were secondary to hypothalamic lesions versus FND.

