Diversity, Equity, and Inclusion
(072) Global CL Psychiatry: a field ripe for exploration

Juan Borda, MD, MSc (he/him/his)
CL Psychiatry Fellow
University of Toronto, Temerty Faculty of Medicine
Toronto, Ontario, Canada- DK
Dilip Koshy, FRCPC
Staff psychiatrist
University of Toronto, Temerty Faculty of Medicine
Toronto, Ontario, Canada 
Josee Lynch, MD CM, FRCPC
Addiction Psychiatrist
University of Toronto, Temerty Faculty of Medicine
Toronto, Ontario, Canada- KF
Kenneth Fung, MD FRCPC MSc DFAPA DFCPA
Professor and Director of Global Mental Health
University of Toronto, Temerty Faculty of Medicine
Toronto, Ontario, Canada
Presenting Author(s)
Co-Author(s)
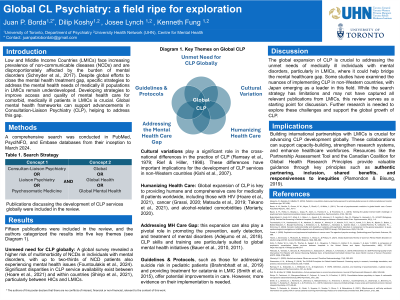
Background/Significance: Low- and middle-income countries (LMICs) are experiencing an increasing prevalence of Non-Communicable Diseases (NCDs) and are disproportionally affected by the growing burden of mental disorders (WHO, 2018). Despite considerable efforts by the global mental health movement to close the treatment gap for people living with mental disorders worldwide, comparatively little attention has been given to the development of strategies to address the mental health needs of medically ill populations in LMICs. From a global mental health perspective, advancements in consultant-liaison (CL) psychiatry may be a promising approach to help address this gap.
Methods: A comprehensive search was conducted in electronic databases including PubMed, PsycINFO, and Embase from inception to March 2024. The search strategy combined keywords related to CL psychiatry with terms for global mental health.
Results: Only two publications explore the relationship between CL psychiatry and global mental health (Bauer, 2010;2011). These publications argued that the skills and training within C–L psychiatry are well-matched to the needs of global mental health work, suggesting a central role for CL psychiatrists in the development of global health strategies, particularly in supporting primary mental health care through a collaborative model. However, these publications did not discuss the challenge of designing and implementing strategies in LMICs to support the mental healthcare of medically ill populations in complex non-psychiatric settings, such as general hospitals, intensive care units, or cancer centres.
Discussion: A global health perspective on CL psychiatry remains largely unexplored. We argue that a global mental health-CL framework will be helpful in designing and implementing strategies to address the mental health treatment gap among medically ill populations of LMICs. As a case study, we will discuss emerging challenges in the process of knowledge translation and capacity building between an alcohol-associated liver disease transplant service in a HIC (UHN-Toronto, Canada) and one of the leading transplant centres in Colombia (Fundacion Valle del Lili – Cali, Colombia). This discussion is informed by the Canadian Coalition of Global Health Research Principles for Global Health Research, including authentic partnering, inclusion, shared benefits, commitment to the future, responsiveness to causes of inequities, and humility (Plamondon, 2019).
Conclusion/Implications: There are current knowledge gaps in how CL psychiatry can be meaningfully employed to address the mental health needs of medically ill populations in LMIC. Use of global health frameworks may guide the advancement of CL psychiatry in global mental health contexts.
References:
Bauer, A. M., Bonilla, P., Grover, M. W., Meyer, F., Riselli, C., & White, L. (2011). The role of psychosomatic medicine in global health care. Current psychiatry reports, 13, 10-17.
Bauer, A. M., Fielke, K., Brayley, J., Araya, M., Alem, A., Frankel, B. L., & Fricchione, G. L. (2010). Tackling the global mental health challenge: a psychosomatic medicine/consultation–liaison psychiatry perspective. Psychosomatics, 51(3), 185-193.
Plamondon, K. M., & Bisung, E. (2019). The CCGHR Principles for Global Health Research: Centering equity in research, knowledge translation, and practice. Social science & medicine, 239, 112530.
WHO. Noncommunicable diseases. 2018. https://www.who.int/news-room/fact sheets/detail/noncommunicable-diseases. Accessed 20 Sept 2020.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: LMICs need to develop strategies to improve the access and quality of mental health care for comorbid medically ill people. From a global mental health perspective, advancements in consultant-liaison (CL) psychiatry may be a promising approach to addressing this gap. Different global mental health frameworks that might be helpful in this endeavour are guided by principles of inclusion, equity, and cultural humility.

