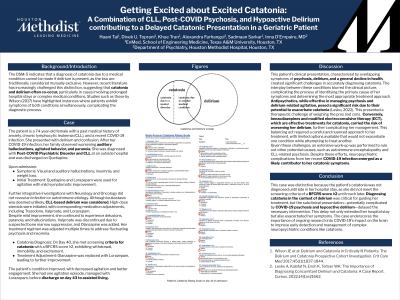
Catatonia
(023) Getting Excited about Excited Catatonia: A Combination of CLL, Post-COVID Psychosis, and Hypoactive Delirium contributing to a Delayed Catatonic Presentation in a Geriatric Patient
Haani Tai
Presenting Author
School of Engineering Medicine, Texas A&M University
Tomball, Texas- DT
Divek Toprani, n/a
Medical Student
School of Engineering Medicine, Texas A&M University
Houston, Texas - KT
Khue Tran, n/a
Medical Student
School of Engineering Medicine, Texas A&M University
Houston, Texas 
Alexandra N. Farhangui, n/a
EnMed Texas A&M Medical Student
School of Engineering Medicine, Texas A&M University
Houston, Texas- ID
Inna D'Empaire, MD
LC Psychiatry
Houston Methodist Hospital
Houston, Texas
Presenting Author(s)
Co-Author(s)
Background/Significance: The DSM-5 states a diagnosis of catatonia due to a medical condition cannot be made in the presence of delirium. Recent literature, however, has shown that these conditions frequently present concurrently in prolonged hospital stays (Wilson, 2017).
Case: Patient is a 74 year-old female with past medical history of anxiety, chronic lymphocytic leukemia (CLL), and recent COVID-19 infection presenting with delirium and confusion. Following her COVID-19 infection a month prior, her family noticed worsening auditory hallucinations, agitated behavior, and paranoia. She was diagnosed with Post-COVID Psychiatric disorder and CLL at an outside hospital and discharged on Seroquel. Upon admission, she experienced visual and auditory hallucinations, insomnia, and weight loss. She was treated with Seroquel and Ativan for agitation, with mild symptomatic improvement. Further integrative investigations with Neurology and Oncology did not reveal infection or autoimmune etiology. Potential CLL-based delirium was suggested, although leukostasis was deemed unlikely. High-dose steroids were initiated empirically, with corresponding medication adjustments, including Trazodone, Depakote, and Ativan. Subsequently she showed mild improvement with continued delusions, paranoia, and hallucinations. Depakote was discontinued from suspected bone marrow suppression, and Zyprexa was added. Her treatment regimen was adjusted multiple times to address her fluctuating psychosis and insomnia. The patient met screening criteria for catatonia for the first time on Day 40 with a BFCRS score ≥2, exhibiting withdrawal, immobility, and excitement, prompting a transition from Zyprexa to Ativan. Her condition continued to improve, with decreased agitation and engagement. She experienced one agitation episode, managed with Ativan, before discharge to assisted living.
Discussion: This patient’s complex clinical presentation with overlapping symptoms of psychosis and delirium along with whole-health deterioration complicated the diagnosis of catatonia. Thus, treatment options were limited as antipsychotics alleviate psychosis and delirium-associated agitation, but can exacerbate catatonia (Lesko, 2022). While benzodiazepines and modified electroconvulsive therapy can be effective for catatonia, delirium may be worsened. In this patient, after extensive work-up to rule out other conditions like autoimmune encephalopathy and CLL psychosis, neuropsychiatric complications due to COVID-19 were concerning for symptoms of catatonia.
Conclusion: This case was unique in that the patient’s catatonia did not meet screening criteria of ≥2 BFCRS categories until late in the hospital stay. Diagnosing catatonia in the setting of delirium was essential for treatment of this patient to alleviate distress and restore independent level of functioning. The subclinical presentation of excited catatonia, potentially complicated by COVID-19 psychosis and elements of hypoactive delirium, delayed necessary intervention that extended the patient’s hospital stay. Ongoing research and innovations are crucial to understanding COVID-19’s neuronal effects.
References:
Wilson JE et al: Delirium and Catatonia in Critically Ill Patients: The Delirium and Catatonia Prospective Cohort Investigation. Crit Care Med 2017;45(11):1837-1844.
Lesko A, Kalafat N, Enoh K, Teltser WK: The Importance of Diagnosing Concomitant Delirium and Catatonia: A Case Report. Cureus. 2022;14(1):e21662.
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: This case report highlights a feature of current consult psychiatric management that disadvantages not only the elderly, but also black Americans who are at a higher risk of catatonia, leading to increasing hospital stays and worsened health outcomes. It highlights the benefits that consult psychiatry can bring in caring for these populations. Our team also reflects a diversity of experiences and background, being led by engineering-medical students interested in urology, radiology, and psychiatry mentored by a C-L attending physician.

