Collaborative and Integrated Care
(054) Collaboration Creates Cures, but Racism Resists Them: Inpatient Psychiatric Patients with First Break Psychosis have Better Outcomes when Medical Workups are Completed, but Who is Receiving the Workup?

Kara Jacobs, MD
Resident Physician
LVHN
Bethlehem, Pennsylvania
Presenting Author(s)
Background/Significance: Psychosis defines a variety of symptoms in which an individual experiences symptom(s) that disrupt their connection with reality [Calabrese 2023]. The first time a patient experiences psychosis is often termed “first episode psychosis” (FEP) [Prakash, 2021]. This original presentation is an integral part of psychiatric care. An estimated 1-3% of people worldwide will experience FEP [Calabrese, 2023]. However, psychosis is not always purely psychiatric in origin [Calabrese, 2023]. FEP is a heterogeneous phenomenon that can greatly influence the diagnosis and alter the course of the stability and outcome of a patient [Prakash, 2021]. FEP can be caused by genetics, traumatic events, substance use, physical illness, medical diseases, medications, or mental health conditions [Prakash, 2021]. Thus, it has been established that performing a medical diagnostic workup is essential for determining the cause of psychosis and improving patient outcomes [Skikic, 2020]. Knowing the etiology of psychosis helps providers treat patients accordingly, so psychosis can be reduced or eliminated and improve patient functioning [Skikic, 2020].
Methods: An analysis of FEP medical workups on inpatient psychiatric patients at Lehigh Valley Health Network – Behavioral Health Unit (LVHN-BHU) is being completed via retrospective chart review. A timeframe of four years (2019-2023) is being evaluated. 318 charts were found to meet criteria. IRB approval was granted. The outcomes of these patients have been collected, evaluating for any possible disparities between age, race, gender, provider, or chief presenting psychotic complaint.
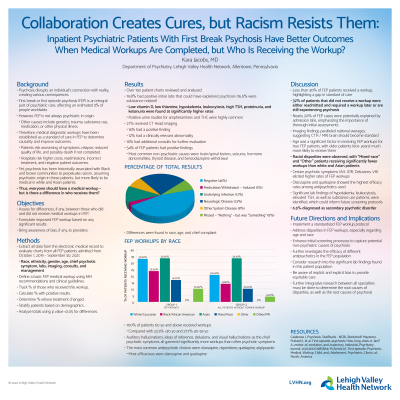
Results: Analysis continues, but is expected to be completed by May 2024. Thus far, the data shows 19% of patients were found to have positive initial admission laboratory studies, suggesting a transient cause of psychosis. Among the most common were substances, pregnancy, and thyroid issues. Of the remaining patients, it appears that only 29% are receiving an FEP medical workup. Of the 29% of patients receiving workups, an astounding 50% of them thus far have been found to have a non-psychiatric cause of psychosis (brain lesions, seizures, and endocrine abnormalities among the most common). Of the remaining 52% that did not receive an FEP workup or had positive initial admission labs, they have varying outcomes. 17% were found to have required medical workup elsewhere. 19% were lost to follow up. 7% were re-admitted for return of symptoms. 9% are doing well and have not required any further intervention. Analysis regarding the above categories is ongoing, but shows disparities between white and Black patients. No significant differences between age, gender, and provider have been found.
Discussion: Half of patients receive FEP workups. The data suggests that collaboration of specialties is essential to non-psychiatric causes of psychosis. Without that, disparities, inequitable care, and gaps in medical education persist.
Conclusion/Implications: Education on psychotic presentations and equitable treatment need to be improved. Further integrative research between all specialties must be done to determine the root causes of disparities, as well as the root causes of psychosis.
References:
Calabrese J. Psychosis. StatPearls - NCBI_Bookshelf. May2023.
Prakash J, et al. First-episode_psychosis: How_long_does_it_last? A_review_of_evolution_and_trajectory. Industrial_Psychiatry Journal. 2021;30(2):198
Skikic M,Arriola JA. First-episode_Psychosis_Medical_Workup. Child_and_Adolescent_Psychiatric_Clinics_of_North_America.
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: This research shows that there are possible disparities among first break psychosis (FEP) medical workups, particularly between white and Black patients. Only 30% of patients are receiving FEP medical workups to begin with, suggesting possible provider burnout or bias, and the majority of these are white patients. By understanding that psychosis has been historically associated with Black and African American communities to perpetuate racism, it is imperative to shine a light on inequitable care, such as assuming psychosis is psychiatric in origin for Black patients, but more likely to be medical in white patients, requiring further workup.

