Psychopharmacology and Toxicology
(137) Clozapine-Induced Urinary Incontinence: A Novel Management Option and Review of the Literature

Connor Hoch, MD
Consultation-Liaison Psychiatry Fellow, PGY-5
Columbia University/New York Presbyterian Hospital
New York, New York- SQ
Seema Quraishi, MD
Division Chief and Fellowship Program Director, Consultation-Liaison Psychiatry
Mount Sinai Beth Israel
New York, New York - DG
Dmitriy Gekhman, MD
Clinical Assistant Professor of Psychiatry
Icahn School of Medicine at Mount Sinai
New York, New York - AS
Ashley Sterchele, MD (she/her/hers)
Medical Director of Integrative Outpatient Services and Associate Program Director
Mount Sinai Beth Israel, New York
Presenting Author(s)
Co-Author(s)
Background/Significance:
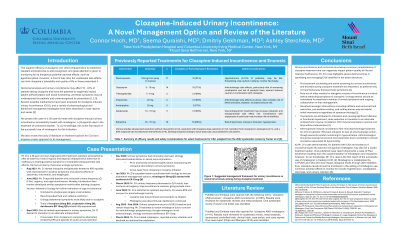
The efficacy of clozapine in treatment-resistant schizophrenia is well-recognized; however, an array of unfavorable side effects can limit its tolerability, with negative impact on whole-person wellbeing. While a lesser-appreciated adverse effect, up to 40% of patients taking clozapine may experience nocturnal enuresis or other urinary incontinence, symptoms associated with negative self-perception and reduced perceived quality of life (Tanzer, 2022; Jönson Ring, 2017; Corrado, 2020).
Case:
We present the case of a 36-year-old male outpatient who developed urinary frequency and urge incontinence with considerable consequent lifestyle limitations months after initiating clozapine for treatment-resistant schizophrenia. Notably, his identical twin brother developed similar urinary symptoms after initiating clozapine for the same indication.
Urologic workup including uroflowmetry and post-void residual was unremarkable, and his overactive bladder symptoms were ultimately attributed to clozapine. Trials of behavioral interventions and antimuscarinics yielded limited benefit in alleviating the patient’s urinary symptoms, and he was unable to tolerate attempts at crosstaper to alternate antipsychotics due to other intolerable medication adverse effects.
Coordinating with urology, the ꞵ3 agonist mirabegron was added with a substantial (~50%) improvement in the patient’s urinary frequency and urgency. Following discontinuation of the patient’s incontinence medications during a later hospitalization, he experienced relapse of his urinary symptoms and was hesitant to restart mirabegron due to concerns related to previous experiences with anticholinergic side effects, despite mirabegron’s minimally anticholinergic profile.
Discussion:
Clozapine-induced urinary incontinence is likely multifactorial in mechanism; case reports and series have described management options of varying success from behavioral interventions and clozapine dose reduction to various pharmacologic approaches across several medication classes, which we will review. The ꞵ3 agonist mirabegron may represent a useful novel management option for clozapine-related urinary incontinence, successful use of which for this indication has to our knowledge not been reported in the literature (Tanzer, 2022).
Conclusion/Implications:
In promoting whole-person healing, it is important for the consultation-liaison psychiatrist to be mindful of potentially lifestyle-limiting adverse effects of medications. Urinary incontinence and enuresis related to clozapine may go underrecognized, yet adversely impact quality of life and carry important implications to patient self-perception and treatment adherence (Jönson Ring, 2017; Corrado, 2020). For clozapine-induced urinary incontinence refractory to behavioral interventions or traditional antimuscarinics, and for which clozapine discontinuation is unfeasible or unsuccessful, mirabegron may represent a novel option for managing urinary symptoms and improving patient quality of life.
References:
[1]Tanzer T, Warren N, McMahon L, Barras M, Kisely S, Brooks E, Wong E, Siskind, D. (2022). Treatment strategies for clozapine-induced nocturnal enuresis and urinary incontinence: A systematic review. CNS Spectrums 2022 Jan; 28:1-2.
[2]Jönson Ring I, Nevéus T, Markström A, Arnrup K, Bazargani F. Nocturnal enuresis impaired children's quality of life and friendships. Acta Paediatr 2017 May;106(5): 806-811.
[3]Corrado B, Giardulli B, Polito F, Aprea S, Lanzano M, Dodaro C. The Impact of Urinary Incontinence on Quality of Life: A Cross-Sectional Study in the Metropolitan City of Naples. Geriatrics (Basel). 2020 Nov; 20;5(4):96.
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: Despite its superior clinical efficacy in treating schizophrenia, the literature demonstrates that clozapine is underutilized in certain demographic groups, for example African Americans, when compared to other groups. Possibly driven in part by concern for medication side effects, this disparity in prescribing practice may place this population at greater risk of adverse illness outcomes. By bringing attention to an under-appreciated clozapine adverse effect and expanding upon previously identified management options, we hope to contribute to the expansion of equitable access to this highly effective medication.

