Collaborative and Integrated Care
(053) Clinician Knowledge, Attitudes, and Confidence Related to the Diagnosis and Management of Somatic Symptom Disorder (SSD) in a General Hospital Setting.

Matthew J. Elton, BBiomedSc BMed FRANZCP
Staff Specialist Psychiatrist
Hunter New England Local Health District
New Lambton Heights, New South Wales, Australia
Matthew J. Elton, BBiomedSc BMed FRANZCP
Staff Specialist Psychiatrist
Hunter New England Local Health District
New Lambton Heights, New South Wales, Australia- SR
Shalini Rajan, n/a
Advanced Trainee, Liaison Psychiatry
Hunter New England Local Health District
New lambton heights, New South Wales, Australia - SR
Shalini Rajan, n/a
Advanced Trainee, Liaison Psychiatry
Hunter New England Local Health District
New lambton heights, New South Wales, Australia
Presenting Author(s)
Co-Author(s)
Background: Somatic Symptom Disorder (SSD) has a high prevalence but is poorly understood and managed in various healthcare settings worldwide (1). Although effective treatments exist (2), many patients are undiagnosed and their underlying psychological conditions often unrecognized and untreated, adding to patient significant symptom-related disability and functional impairment. Diagnostic terminology to describe such conditions in the interface between psychiatry and medicine has also been challenging. This pilot survey of clinicians’ perceptions about SSD in an Australian general hospital setting aimed to explore the association between perceptions of SSD and specific clinician characteristics, to inform future service development initiatives.
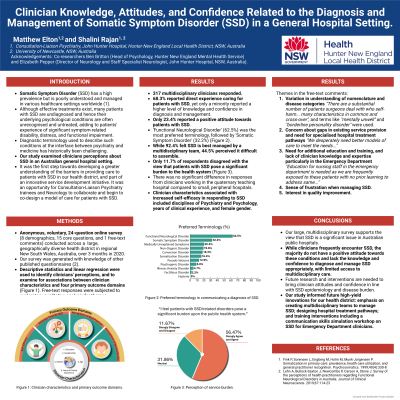
Methods: Anonymous, voluntary, 25-question online survey conducted across a large, geographically diverse health district in regional New South Wales, Australia. Descriptive statistics and linear regression were used to identify clinicians' perceptions, and examine associations between clinician characteristics (age, gender, discipline, years of clinical experience, and hospital site) and primary outcome domains of 1) self-efficacy in responding to SSD (knowledge and confidence), 2) attitudes towards SSD, 3) perceptions of best practice, and 4) perceptions of service burden.
Results: n=317 multidisciplinary clinicians. 68.3% reported direct experience in caring for SSD patients, yet only a minority reported a higher level of knowledge and confidence in diagnosis and management. 23.4% reported a positive attitude toward working with these patients. Only 19.6% of doctors rarely or never encountered SSD in their public inpatient practice, and only 23.4% rarely or never in their public outpatient practice. Only 11.7% disagreed with the view that patients with SSD pose a significant burden to the health system. Half of respondents' reported difficulty assembling a multidisciplinary team to manage SSD. No significant difference was detected between responses from clinicians in the quaternary teaching hospital, and smaller peripheral hospitals. Clinician characteristics associated with increased self-efficacy in responding to SSD included disciplines of psychiatry and psychology, years of clinical experience, and female gender.
Discussion: This study endorses SDD as a significant issue in Australian public hospitals. Clinicians frequently encounter patients with SSD yet lack the knowledge and confidence to diagnose and manage such conditions appropriately, with limited access to multidisciplinary care. Only a minority of clinicians consider working with patients with SSD rewarding. SSD is a significant issue irrespective of hospital size or availability of resources. Patients with SSD experience significant distress and disability, which is compounded by clinician perceptions of health system burden.
Conclusion: This study was part of an innovative service development initiative and an opportunity for Consultation-Liaison Psychiatry trainees and Neurology to collaborate and begin to co-design a model of care for patients with SSD within our health district. It has identified high-yield areas for future intervention such as an emphasis on multidisciplinary team development; creating hospital and community health pathways; and training recommendations.
References:
1) Fink P, Sørensen L, Engberg M, Holm M, Munk-Jørgensen P. Somatization in primary care: prevalence, health care utilization, and general practitioner recognition. Psychosomatics. 1999;40(4):330-8
2) Henningsen P, Zipfel S, Sattel H, Creed F. Management of functional somatic syndromes and bodily distress. Psychotherapy and Psychosomatics. 2018;87(1):12-31
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: Patients with SSD experience significant levels of symptom-related disability and functional impairment. SSD also accounts for disproportionately high healthcare resource consumption, with patients utilizing primary care at two-fold greater rates and having three-fold greater hospital bed days than aged-matched controls. Despite poor health outcomes and high healthcare utilization, effective hospital models of care are generally not implemented or available locally. Our pilot survey was a first step in our health district towards bridging this gap. The authors also include diversity in career stage including psychiatry trainee and early career psychiatrist, from a regional Australian setting, in collaboration with neurology colleagues.

