Cardiology
(006) Can We Be Too Happy? A Variant of Broken Heart Syndrome

Daniel Fisher, MD
Resident
Wright State University
Oakwood, Ohio- RB
Robert Buntyn, DO
Resident Physician
Boonshoft School of Medicine, Wright State University
Fairborn, Ohio - SA
Saipriya Ayyar, n/a
Medical Student
Boonshoft School of Medicine, Wright State University
Dayton, Ohio - VM
Vaskar Mukerji, MBBS
Professor
Boonshoft School of Medicine, Wright State University
Dayton, Ohio
Presenting Author(s)
Co-Author(s)
Background/Significance:
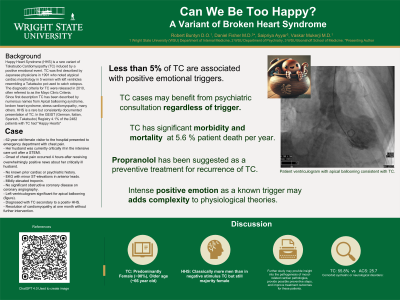
Happy Heart Syndrome (HHS) is a rare variant of Takotsubo cardiomyopathy (TC) associated with intense positive emotion rather than heartbreak. Here we present a case and discuss a possible role for psychiatric consultation.
Case:
A 62-year-old woman had come in to the hospital to see her husband who was in critical condition in the ICU following a major heart attack the day before. He had undergone percutaneous intervention which was complicated by ventricular fibrillation. The wife was told that he was critically ill. The following day, when she was visiting, she was informed that her husband had made a remarkable recovery and was doing exceptionally well after his heart attack. She was overcome with joy, and with tears flowing from her eyes, and thanked the care team.
Four hours later, she experienced chest pain and dypsnea for which she was taken to the Emergency Department (ED). She was previously in good health with no history of cardiac or psychiatric problems. In the ED, her electrocardiogram showed ST elevations in the anterior leads with a serum troponin elevation suggestive of acute myocardial infarction. She was immediately taken for cardiac catheterization, but surprisingly, her angiography revealed no significant blockages. Left ventriculography demonstrated the characteristic apical ballooning of TC. Her case of TC required only monitoring and outpatient follow-up. Her symptoms resolved spontaneously, and her one-month follow-up showed that her left ventricular dysfunction had normalized.
Discussion:
TC has been commonly referred to as the Broken Heart Syndrome. A recent review of an international registry of stress-induced cardiomyopathy cases reported that less than five percent of cases were consistent with HHS (Stiermaier, 2022). Traditionally, the pathophysiology of TC was thought to be due to a catecholamine surge from intense negative emotion (Nayeri, 2018). Now, both positive and negative emotions have been recognized.
There is a strong association between pre-existing anxiety, mood-spectrum disorders, and TC. Our patient had no recorded history of psychiatric illness at the time of her TC diagnosis. A previous case report proposed propranolol as a preventive therapy for recurrence of traditional TC (Costin, 2011). Although this could be beneficial for both the psychiatric and physiologic components of traditional TC associated with a “tragic event”, a “happy event” may not respond in the same way. Suppression of happiness is generally not a desirable long-term treatment. No known study has focused on the treatment of underlying psychiatric conditions in the long-term management of TC.
Conclusion/Implications:
Patients with TC may benefit from psychiatric consultation regardless of trigger. Increased awareness and data capture for HHS may be accomplished through proactive psychiatric consultation strategies. Further study may provide insight into the pathogenesis of mood-related cardiac pathologies, provide possible preventive steps, and improve treatment outcomes.
References:
Costin et al (2011). A Psychosomatic Perspective on Takotsubo Cardiomyopathy: A Case Report. The Primary Care Companion to CNS Disorders, 13(2), PCC.10br00980
Nayeri et al (2018). Psychiatric Illness in Takotsubo (Stress) Cardiomyopathy: A Review. Psychosomatics,59(3),220–226.
Stiermaier et al. (2022). Happy Heart Syndrome. JACC: Heart Failure,10(7),459–466.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: This case study and abstract was a multidisciplinary collaboration between residents and students studying psychiatry, internal medicine, and cardiology. The cross-discipline involvement of this case allowed for increased diversity in exposure of cardiology phenomena to a psychiatry trainee and for the introduction of psychosomatic medicine to an internal medicine trainee. Additionally, a medical student who has not yet decided which field of medicine they will pursue residency training in was able to study a unique disease presentation and explore the implications of the ambiguity in treatment of rare disease.

