Catatonia
(025) Multidisciplinary Management of Malignant Catatonia in a Geriatric Patient: A Consultation-Liaison Psychiatry Case Report

Bishoy Abdelmalik (he/him/his)
Medical Student
UF College of Medicine
Gainesville, Florida
Diego Nolasco, MD
Resident Physician
University of Florida College of Medicine
Gainesville, Florida- BC
Brent R. Carr, MD DFAPA
Associate Professor
University of Florida
Gainesville, Florida
Presenting Author(s)
Co-Author(s)
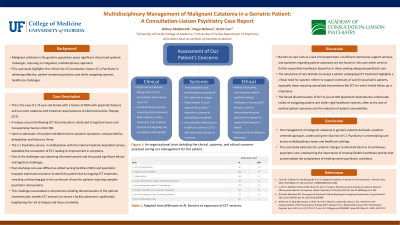
Background/Significance: Malignant catatonia in the geriatric population poses significant clinical and systemic challenges, necessitating an integrated, multidisciplinary approach. This case study illuminates the critical role of Consultation-Liaison (C-L) Psychiatry in addressing the intricate interplay of psychiatric treatment efficacy, systemic healthcare barriers, and patient-centered care coordination. The complexities encountered in managing a geriatric patient with malignant catatonia underscore the importance of holistic, patient-focused strategies in navigating healthcare systems and treatment modalities.
Case Description: We present the case of a 73-year-old female with a historical responsiveness to Electroconvulsive Therapy (ECT) for catatonia. A relapse occurred following ECT discontinuation, attributed to logistical issues and transportation barriers. Upon re-admission, the patient exhibited severe catatonic symptoms, compounded by dehydration and failure to thrive. The C-L Psychiatry service, in collaboration with the internal medicine hospitalist service, expedited the resumption of ECT. Obtaining informed consent posed significant ethical and logistical challenges due to the patient's fluctuating consciousness. Despite initial symptomatic improvement with ECT, the patient faced substantial systemic obstacles related to post-discharge care. Skilled Nursing Facilities (SNFs) and psychiatric hospitals expressed reluctance to admit the patient due to ongoing ECT treatment, revealing a distressing gap in the continuum of care for patients requiring complex psychiatric interventions. This impasse necessitated a compromise: discontinuation of the optimal treatment plan (weekly ECT sessions) to secure a facility placement, significantly heightening the risk of relapse and future morbidity.
Discussion: This case emphasizes the multifaceted dilemmas faced by the C-L Psychiatry team, spanning clinical, ethical, and systemic domains. Barriers to care such as a lack of transportation, insufficient community support services, and questions regarding patient autonomy are key factors in this case which serve to further exacerbate healthcare disparities in those seeking adequate psychiatric care. Additionally, the reluctance of care facilities to accept a patient undergoing ECT treatment highlights a critical need for systemic reform to support continuity of care for psychiatric patients, especially those requiring specialized interventions like ECT for which timely follow-up is imperative. The forced discontinuation of ECT to secure SNF placement illustrates the stark realities of navigating patient care within rigid healthcare systems, often at the cost of optimal patient outcomes and the reduction of patient comorbidities.
Conclusion/Implications: The management of malignant catatonia in geriatric patients demands a nuanced, patient-centered approach, underscoring the vital role of C-L Psychiatry in orchestrating care across multidisciplinary teams and healthcare settings. This case study advocates for systemic changes to eliminate barriers to continuous psychiatric care, emphasizing the importance of creating flexible healthcare policies that accommodate the complexities of treating severe psychiatric conditions. Bridging the gap between psychiatric treatment needs and healthcare system capabilities is essential for improving outcomes and quality of life for this vulnerable population.
References:
1) Lloyd JR, Silverman ER, Kugler JL, Cooper JJ. Electroconvulsive Therapy for Patients with Catatonia: Current Perspectives. Neuropsychiatr Dis Treat. 2020;16:2191-2208. Published 2020 Sep 25. doi:10.2147/NDT.S231573
2) Wilkinson ST, Kitay BM, Harper A, et al. Barriers to the Implementation of Electroconvulsive Therapy (ECT): Results From a Nationwide Survey of ECT Practitioners. Psychiatr Serv. 2021;72(7):752-757. doi:10.1176/appi.ps.202000387
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: To start, we believe this submission does advance diversity, equity, and inclusion as our authors are in all different levels of training and are from diverse cultural backgrounds: the medical student as the first author and presenter; a psychiatry resident as a coauthor; and a psychiatry attending as the corresponding author. Furthermore, a core component of our submission is in addressing specific health inequities and disparities, such as a barrier to transportation and insufficient community services, encountered by our patient which ultimately affected their ability to achieve adequate care.

