COVID-19
(003) Long-Covid Consultation Clinic: An Integrated Care Model and Exploration of Current Treatment Modalities.
Michael Stephen La Sala, DO , MSc
Director of Consultation - Liaison Psychiatry
Florida Atlantic University
Weston, Florida- BB
Brian Bronson, MD (he/him/his)
Professor of Clinical Psychiatry & Behavioral Health
Stony Brook University
Stony Brook, New York
Presenting Author(s)
Co-Author(s)
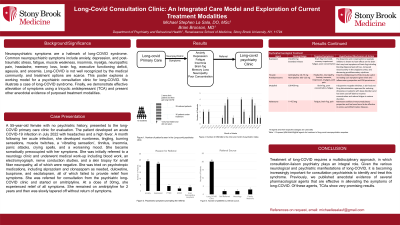
Background/Significance: Neuropsychiatric symptoms are a hallmark of long-COVID syndrome. Common neuropsychiatric symptoms include anxiety, depression, and post-traumatic stress, fatigue, muscle weakness, insomnia, myalgia, neuropathic pain, headache, memory loss, brain fog, executive functioning deficit, ageusia, and anosmia [Davis et. al., 2021]. Long-COVID is not well recognized by the medical community, and treatment options are scarce. This poster explores a working model for a psychiatric consultation clinic for long-COVID. We illustrate a case of long-COVID syndrome. Finally, we demonstrate effective alleviation of symptoms using a tricyclic antidepressant (TCA).
Case: A 55-year-old female with no psychiatric history, presented to the long-COVID primary care clinic for evaluation. The patient developed an acute COVID-19 infection in July 2022 with headaches and a high fever. A month following her acute infection, she developed numbness, tingling, burning sensations, muscle twitches, a ‘vibrating sensation’, tinnitus, insomnia, panic attacks, crying spells, and a worsening mood. She became somatically preoccupied with her symptoms. She was initially referred to a neurology clinic and underwent medical work-up including blood work, an electromyograph, nerve conduction studies, and a skin biopsy for small fiber neuropathy, all of which were negative. She was tried on psychotropic medications, including alprazolam and clonazepam as needed, duloxetine, buspirone, and escitalopram, all of which failed to provide relief from symptoms. She was referred for consultation from the psychiatric long-COVID clinic and started on amitriptyline. At a dose of 30mg, she experienced relief of all symptoms. She remains on amitriptyline to this day and is symptom-free.
Results: From August 2021 to May 2023, 31 patients were seen by the psychiatric long-COVID clinic. Of these, 20 patients were referred from the primary care long-COVID clinic, 2 self-referred, 2 from neurology, 3 from a primary care physician in the community and 3 were already part of the clinic. 24 patients were referred for anxiety, 22 for depression and 9 for PTSD and/or brain fog. Trials of several medications were attempted, but only a few demonstrated efficacy. This case report demonstrates effective treatment using a TCA.
Discussion: Treatment of long-COVID requires a multidisciplinary approach, in which consultation-liaison psychiatry plays an integral role. Given the various neurological and psychiatric manifestations of long-COVID, it is becoming increasingly important for consultation psychiatrists to identify and treat this syndrome. Previously, we published anecdotal evidence of several pharmacological agents that are effective in alleviating the symptoms of long-COVID [Reinfeld, 2023]. Of these agents, TCAs show very promising results [La Sala, 2023].
Conclusion: We demonstrate a model for a consultation psychiatry long-COVID clinic, illustrated with an unpublished case of neuropsychiatric sequalae of long-COVID effectively treated with a TCA.
References:
< !1. Davis HE, et al. Characterizing long-COVID in an international cohort: 7months of symptoms and their impact. EClinicalMedicine. 2021;38:101019.
< 2. Reinfeld S, La Sala M. Exploring therapeutic approaches for long COVID neuropsychiatric sequelae: current understanding and potential strategies. Prim Care Companion CNS Disord. 2023;25(5):23br03592.
< !3. La Sala MS, et. al. Treatment of Long-COVID Neuropsychiatric Sequelae Using Tricyclic Antidepressants: A Case Series. J Clin Psychopharmacol. 2023 Sep-Oct 01;43(5):458-460.
Presentation Eligibility: Data presented in this poster has not been published, presented, or submitted to any other entity.
Diversity, Equity, and Inclusion: The consultation psychiatry long-covid model provides psychiatric care to patients from historically marginalized populations. The data presented here includes the treatment of patients from various ethnic and socioeconomic backgrounds. These individuals include African Americans, Hispanics, Caucasians, and those below the poverty line. Stony Brook University Hospital provides access to care for patients of all socioeconomic statuses. This clinic is part of a multidisciplinary care team that also provides various medical resources to patients from historically marginalized, underserved, and vulnerable populations. Finally, we are currently seeking federal funding in an effort to increase access to care for rural populations.

