Diversity, Equity, and Inclusion
(076) Self-Orchiectomy in a Non-psychotic Non-binary Patient

Caitlin McCarthy, MD (she/her/hers)
Consultation-Liaison Psychiatry Fellow
Medical College of Wisconsin
Milwaukee, Wisconsin- SL
Sara Lindeke, MD
Assistant Professor
Medical College of Wisconsin
Wauwatosa, Wisconsin
Presenting Author(s)
Co-Author(s)
Background/Significance: Self-orchiectomy is a rare occurrence primarily documented in the context of psychosis (Garofalo et al., 2018; Kalin, 1979; Lupu et al., 2021). For transgender or non-binary patients with limited access to gender-affirming healthcare, self-orchiectomy may feel like a last resort. We present a case of self-orchiectomy in a non-binary patient without acute psychosis who demonstrated capacity for refusing urological re-attachment of testicles.
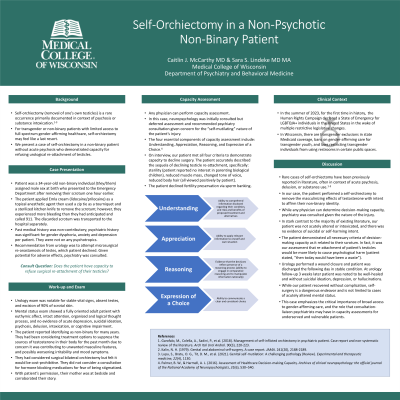
Case: A 34-year-old non-binary individual assigned male sex at birth presented to the Emergency Department after removing their scrotum several hours earlier at home. The patient removed their testicles to eliminate a source of testosterone. The patient used a zip tie as a tourniquet and a kitchen knife to remove the scrotum but experienced excessive bleeding and called 911. Psychiatry was consulted to assess decision-making capacity to refuse testicle re-attachment. The patient was fully oriented with intact attention, organized thought process, and no evidence of psychosis, delusion, or substance use; they denied depression or suicidal ideation and affect was euthymic and mood-congruent. The patient verbalized necessary criterion for decision-making capacity. Urology performed a wound closure and patient was discharged the following day.
Discussion: While rare cases of self-orchiectomy have been reported in literature, the vast majority are in context of psychosis, delusion, or substance use (Garofalo et al., 2018; Kalin, 1979; Lupu et al., 2021). We present a non-binary individual who performed a self-orchiectomy to remove masculinizing effects of testosterone. Urology consulted psychiatry to determine decision-making capacity. The patient was not psychotic, manic, intoxicated, or suicidal. The criteria of decision-making capacity include: understanding of the condition including risks, benefits, and alternatives, ability to appreciate and apply all relevant information, clear reasoning, and expression of a consistent choice (Palmer & Harmell, 2016). Our patient described the sequela of losing their testicles (including sterility, reduced muscle mass, higher voice, and less body hair) and expressed the choice to refuse testicle re-attachment.
Conclusion/Implications: We present a unique case of a non-psychotic, non-binary individual who performed self-orchiectomy to alleviate gender dysphoria. While our patient recovered without issue, self-surgery is a dangerous endeavor. In summer 2023, the Human Rights Campaign declared a state of emergency for LGBTQ+ individuals in the United States in the wake of multiple legislative changes restricting access to inclusive healthcare. This case illustrates that self-orchiectomy is not limited to cases of psychosis or substance use and emphasizes the critical importance of broad access to gender-affirming care.
References:
1. Garofalo, M., Colella, A., Sadini, P., et al. (2018). Management of self-inflicted orchiectomy in psychiatric patient. Case report and non-systematic review of the literature. Arch Ital Urol Androl. 90(3), 220-223.
2. Kalin, N. H. (1979). Genital and abdominal self-surgery. A case report. JAMA. 241(20), 2188-2189.
3. Lupu, S., Bratu, O. G., Tit, D. M., t al. (2021). Genital self-mutilation: A challenging pathology (Review). Experimental and therapeutic medicine, 22(4), 1130.
4. Palmer, B. W., & Harmell, A. L. (2016). Assessment of Healthcare Decision-making Capacity. Archives of clinical neuropsychology: the official journal of the National Academy of Neuropsychologists, 31(6), 530–540.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: We present an interesting case of a non-binary patient who performed a self-orchiectomy at home. In contrast with much of the literature, the patient was not psychotic, and the actions were not suicidal in nature. The psychiatry team played an important role in liaising with the urology faculty, as the patient declined testicle re-attachment and urology requested an assessment of decision-making capacity. Our case demonstrates the critical need for access to inclusive and gender-affirming care in the United States, and emphasizes the importance of collaboration between specialties to act in the best interests of the patient.

