Neurocognitive Disorders and Neuropsychiatry
(098) Responsive Neurostimulation Associated Panic Symptoms: A Case Report
Robyn Bartel, MD
Resident Physician
University of New Mexico School of Medicine
Albuquerque, New Mexico
Tessa Olmstead, MD
Resident Physician
University of New Mexico School of Medicine
Albuquerque, New Mexico- GN
Gregory Nikogosyan, DO
Assistant Professor of Psychiatry
University of New Mexico School of Medicine
Albuquerque, New Mexico
Presenting Author(s)
Co-Author(s)
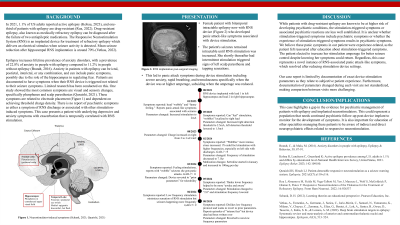
Background/Significance: In 2021, 1.1% of US adults reported active epilepsy (Kobau, 2023), and one-third of patients with epilepsy are drug-resistant (Roa, 2022). The Responsive Neurostimulation System (RNS) is an implanted device for treatment of refractory epilepsy which delivers an electrical stimulus when seizure activity is detected. Epilepsy increases lifetime prevalence of anxiety disorders, posing a risk factor for panic attacks. Patients are documented to have symptoms when their RNS device is triggered not related to their seizure symptoms. Limited research has been conducted on this. One study showed the most common signs are visual and sensory changes, specifically phosphenes and scalp paresthesias (Quraishi, 2021).
Case: Here, we discuss a case study focusing on a female patient with bitemporal intractable epilepsy now with RNS device who developed panic attack-like symptoms associated with device stimulation. Consent was obtained from the patient to complete this case presentation. This patient’s RNS had target placement with bilateral hippocampal depth electrodes. The patient's seizures remained intractable until RNS stimulation was increased. She shortly thereafter had intermittent stimulation triggered signs of left scalp paresthesia and tapping sensations. This led to panic attack symptoms during device stimulation including severe anxiety, rapid breathing, and tremulousness specifically when the device was at higher amperage, subsiding when the amperage was reduced. In a literature search, there is no report of psychiatric symptoms as either a symptom of RNS discharge or associated with other stimulation-induced symptoms. This case presents a patient with underlying depressive and anxiety symptoms, with an exacerbation that is temporally correlated with RNS stimulation.
Discussion: While patients with drug-resistant epilepsy are known to be at higher risk of developing psychiatric conditions, the stimulation-triggered symptoms or associated psychiatric reactions are less well established. It is unclear whether stimulation-triggered signs include psychiatric symptoms or whether the experience of stimulation-triggered signs results in psychiatric symptoms. We believe these panic symptoms in our patient were experience-related, as the patient felt reassured after education about stimulation-triggered signs. The patient elected to increase her stimulation amperage for better seizure control despite knowing her symptoms could return. Regardless, this case represents a novel instance of RNS-associated panic attack-like symptoms, which resolved after reducing stimulation device settings.
Conclusion/Implications: This case highlights a gap in the evidence for psychiatric management of these patients. This could represent a population that needs continued psychiatric follow-up post-device implant to monitor for the development of symptoms. It is also important for education of other specialties managing these patients to be aware of indirect and direct neuropsychiatric effects related to responsive neurostimulation.
References:
Kobau R, Luncheon C, Greenlund K: Active epilepsy prevalence among U.S. adults is 1.1% and differs by educational level-National Health Interview Survey, United States, 2021. Epilepsy Behav 2023; 142:109180.
Roa J, Abramova M, Fields M, Vega-Talbott M, Yoo J, Marcuse L, Wolf S, McGoldrick P, Ghatan S, Panov F: Responsive Neurostimulation of the Thalamus for the Treatment of Refractory Epilepsy. Front Hum Neurosci. 2022; 16:926337
Quraishi IH, Hirsch LJ: Patient-detectable responsive neurostimulation as a seizure warning system. Epilepsia. 2021;62(7):e110-e116.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: Our case represents a confluence of factors which visibly and invisibly impact patient experience. Structurally our hospital exists in an under-resourced location, reducing accessibility to care. There is a factor of intersectionality as the patient is female-identified, diagnosed with a psychiatric disorder, and has epilepsy, which have collectively led to historical stigma and delay in treatment. Additionally, among patients with epilepsy, comorbid psychiatric disorders such as panic disorder are frequently missed, further adding to inequity of care.
Devinsky O. Psychiatric comorbidity in patients with epilepsy: implications for diagnosis and treatment. Epilepsy Behav. 2003;4 Suppl 4:S2-S10.

