Catatonia
(030) Resolving catatonia with vitamin infusions? Late-onset cobalamin C deficiency diagnosed through medical evaluation for progressive catatonia

Brandon Hamm, MD, MS (he/him/his)
Assistant Professor
Northwestern University
Chicago, Illinois- VH
Veronika Hanko, MD
CL Psychiatrist
Northwestern University
Chicago, Illinois
Presenting Author(s)
Co-Author(s)
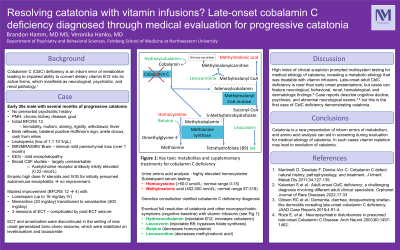
Cobalamin C deficiency is an inborn error of metabolism leading to impaired ability to convert dietary vitamin B12 into its active forms, which manifests as neurological, psychiatric, and renal pathology (Martinelli 2010). We are reporting a young adult presenting with catatonia, prompting medical evaluation that led to diagnosis of late-onset CblC deficiency.
Case:
An early 20s male with no premorbid psychiatric history, but history of chronic kidney disease and gout, presented after months of progressively worsening catatonia. Initial Bush Francis Catatonia Rating Scale (BFCRS) was 12 (immobility, mutism, staring, rigidity, withdrawal, fever). Physical exam demonstrated brisk reflexes, bilateral positive Hoffman’s sign and ankle clonus, as well as a rash from mites. Serum showed leukopenia (low of 1.1 10ˆ3/µL). The initial MRI Brain was unremarkable, but MRI/MRA/MRV Brain a month later demonstrated interval mild parenchymal loss. EEG showed mild encephalopathy, broad CSF studies were unremarkable, and serum acetylcholine receptor antibody was mildly elevated (0.22 nmol/L).
Empiric courses of high dose IV steroids and IVIG for initially presumed autoimmune encephalitis were without meaningful improvement. Modest improvement in catatonia symptoms (BFCRS to 4) was achieved with trials of lorazepam (16 mg/day IV), memantine (20 mg/day) transitioned to amantadine (400 mg/day), and 2 sessions of ECT. ECT and amantadine were discontinued in the setting of new onset generalized tonic clonic seizures, which were stabilized on levetiracetam and lacosamide.
Urine amino acid analysis eventually resulted, showing highly elevated homocysteine, with subsequent serum homocysteine ( >50.0 umol/L; normal range 0-15) and methylmalonic acid (452,000 nmol/L; normal range 87-318) levels demonstrating severe elevation. Genetics consultation clarified diagnosis of CblC deficiency. He was started on leucovorin, betaine, levocarnitine, hydroxocobalamin with eventual full resolution of catatonia and other neuropsychiatric symptoms (cognitive baseline).
Discussion:
High index of clinical suspicion prompted multisystem testing for medical etiology of catatonia, revealing a metabolic etiology that was treatable with vitamin infusions. Late-onset adult CblC deficiency is rarer than early onset presentations, but cases can feature neurological, behavioral, renal, hematological, and dermatologic findings (Kalantari 2022). Case reports describe cognitive decline, psychosis, and abnormal neurological exams (Roze 2003; Gibson 2018), but this is the first case of CblC deficiency demonstrating catatonia.
Conclusion:
Catatonia is a rare presentation of inborn errors of metabolism, and amino acid analysis can aid in screening during evaluation for medical etiology of catatonia. In such cases vitamin repletion may lead to resolution of catatonia.
References:
Gibson RC et al.: Dementia, diarrhea, desquamating shellac-like dermatitis revealing late-onset cobalamin C deficiency. JAAD Case Reports 2018;4:91-4.
Kalantari S et al.: Adult-onset CblC deficiency: a challenging diagnosis involving different adult clinical specialists. Orphanet Journal of Rare Diseases 2022;17:33
Martinelli D, Deodato F, Dionisi-Vici C: Cobalamin C defect: natural history, pathophysiology, and treatment. J Inherit Metab Dis 2011;34:127-135.
Roze E, et al.: Neuropsychiatric disturbances in presumed late-onset Cobalamin C Disease. Arch Neurol 2003;60:1457-1462.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: The patient in this case report was Hispanic and with low socioeconomic status. His opportunities in life were challenged by undiagnosed metabolic disorder and and he dropped out of college due to developing neuropsychiatric symptoms progressing to catatonia. Accurate diagnosis and appropriate management restored his baseline cognition, and with it opportunity to resume education.

