Collaborative and Integrated Care
(066) Reducing Inequity in Accessing Mental Health Care in Marginalized Groups by Embedding Psychology Residents in an Inpatient Pediatric Service
- TD
Thom Dunn, PhD
Staff Psychologist
Denver Health/U of Northern CO
Denver, Colorado - TD
Thom Dunn, PhD
Staff Psychologist
Denver Health/U of Northern CO
Denver, Colorado - KN
Ken Novoa, MD, FACLP (he/him/his)
Vice Chair - Behavioral Health Services
Denver Health Medical Center
Denver, Colorado - KN
Ken Novoa, MD, FACLP (he/him/his)
Vice Chair - Behavioral Health Services
Denver Health Medical Center
Denver, Colorado 
Emili Pickenpaugh, PhD, Licensed Psychologist (she/her/hers)
Psychologist
Denver Health
Denver, Colorado
Emili Pickenpaugh, PhD, Licensed Psychologist (she/her/hers)
Psychologist
Denver Health
Denver, Colorado
Presenting Author(s)
Co-Author(s)
Background
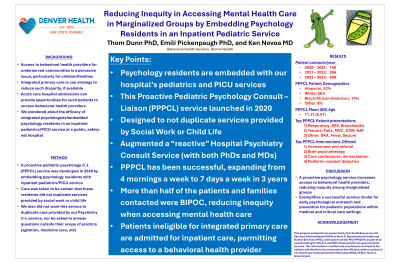
Access to behavioral health providers for underserved communities is a pervasive issue, particularly by children/families(1). Integrated primary care is one strategy to reduce such disparity(2). However, many low-income, migrant, and other marginalized groups have no primary care(3). Although they often are admitted to medical/surgical services providing opportunities to be contacted by behavioral health providers. We wondered about the efficacy of integrated psychologists/embedded psychology residents in an inpatient pediatrics/PICU service at a public, safety-net hospital.
Method
A proactive pediatric psychology C-L (PPPCL) service was developed in the 2020 embedding psychology residents with inpatient pediatrics/PICU service. This pilot program involved two psychology residents, four mornings a week. Care was taken to be certain that these residents did not duplicate services provided by social work or child life. We also did not want this service to duplicate care provided by our Psychiatry C-L service, nor be asked to answer questions outside their scope of practice.
Results
The service was well received by both patients/families and pediatrics staff, faculty, and residents. The program was expanded to residents, 5 days a week in Year 2, and to 3 residents, 7 days a week in Year 3.
Program Consults by year:
Year 1: 158
Year 2: 294
Year 3: 409
Across all years, the majority of patients encountered were Hispanic, Black, Asian, or Native American. A majority either had no insurance or were covered by Medicaid.
The most common medical presentations were:
1) Respiratory: Asthma/RSV/Bronchiolitis/Hypoxia/Hypoxemia
2) Trauma: Falls, MVC, GSW, NAT
3) Other: DKA, Fever, Seizure
Top interventions offered:
1) Assessment and referrals
2) Brief psychotherapy and coping
3) Other: Care conferences, mediating conflict, de-escalation
Psychiatry C-L Consults by year:
Year 1: 115
Year 2: 72
Year 3: 65
Discussion
A proactive pediatric psychology consult-liaison service was successfully established and a majority of patient contacts were to those from under-represented groups. Such contacts have been shown to shorten length of stay(4) and reduce rates of readmission(5). There was a decline in the number of consults placed to a traditional Psychiatry C-L service. Services who rely on RVUs may find this disquieting. However, as was the case in our hospital, provided some relief to a busy C-L service who had to triage cases.
Conclusion/Implications
General hospitals with a pediatric commitment, may be able to increase access to behavioral health to marginalized groups by embedding pediatric psychology residents in the pediatric services.
References
1. Bringewatt et al. Falling through the cracks: Child Youth Serv Rev. 2010 Oct 1;32(10):1291-9.
2. Hodgkinson et al. Improving mental health access for low-income children and families in the primary care setting. Pediatrics. 2017 Jan 1;139(1).
3. Dias S et al. Health policies, patterns and barriers to migrants’ access to primary health care. Access pri care prevent health serv. 2018:99-109.
4.Oldham et al. A systematic review of proactive psychiatric consultation on hospital length of stay. General hospital psychiatry. 2019 Sep 1;60:120-6.
5.Lanvin et al. Early liaison psychiatry consultations and general hospital readmission. General Hospital Psychiatry. 2022 Jul 1;77:29-36.
Presentation Eligibility: This work has not been accepted for publication.
Diversity, Equity, and Inclusion: The submission details a method for other hospitals to follow to increase access to behavioral health specialists to groups who have inequitable access to mental health care.

