Psycho-Oncology and Palliative Care
(123) Psychopharmacologic Considerations in End-of-Life Planning for Patients with SMI: A Case Report
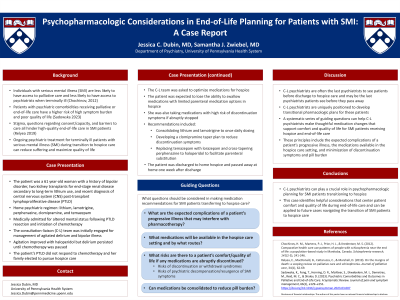

Jessica Dubin, MD
Resident Physician
University of Pennsylvania
Philadelphia, Pennsylvania
Samantha Zwiebel, MD (she/her/hers)
Assistant Professor of Clinical Psychiatry
University of Pennsylvania Perelman School of Medicine
Philadelphia, Pennsylvania
Presenting Author(s)
Co-Author(s)
Background:
Ongoing psychiatric treatment for terminally ill patients with serious mental illness (SMI) during transition to hospice care can reduce suffering and maximize quality of life. We present a case of bipolar disorder in a patient with CNS post-transplant lymphoproliferative disease (PTLD) during transition to hospice care and discuss considerations used to guide pharmacologic decision-making. A 61 year-old woman with a history of bipolar disorder, two kidney transplants following end-stage renal disease secondary to lithium use, and recent diagnosis and resection of CNS PTLD was admitted for worsening altered mental status. The patient had a history of bipolar disorder on a stable regimen of lithium, lamotrigine, perphenazine, clomipramine, and temazepam. Psychiatry was consulted for management of agitated delirium and underlying bipolar illness. Her cancer failed to respond to further treatment and family subsequently elected to pursue hospice care. The consultation-liaison (C-L) team was asked to optimize her medications for hospice while maintaining her psychiatric stability. Specific considerations included that the patient was expected to lose ability to take oral medications, was taking medications likely to cause discontinuation symptoms if abruptly stopped, and would have limited parenteral medication options in hospice care. Discharge medication recommendations included consolidating lithium and lamotrigine to once daily dosing and tapering clomipramine over several weeks to reduce discontinuation symptoms. Recommendations also included replacing temazepam with lorazepam and cross-tapering perphenazine to haloperidol to facilitate anticipated eventual parenteral substitution. The patient was subsequently discharged to home hospice and ultimately passed away at home one week after hospital discharge. Once patients with SMI are discharged to end-of-life care, they are significantly less likely to see a psychiatrist than they were previously (Chochinov, 2012). C-L psychiatrists are therefore frequently the last psychiatrists to see medically hospitalized patients before they are discharged to hospice care, and may be the last psychiatrists that these patients see before they pass away. While C-L psychiatrists are uniquely positioned to develop a transitional pharmacologic plan for these patients, there is sparse guidance on how to do so. We propose a series of considerations that can be helpful in making these medication recommendations. These include the expected complications of a patient’s progressive illness, the medications available in the hospice care setting, and minimization of discontinuation symptoms and pill burden. In this patient’s case, the psychiatry team was able to provide recommendations tailored to her anticipated hospice needs and end-of-life goals. C-L psychiatrists can play a crucial role in psychopharmacologic planning for SMI patients transitioning to hospice. This case identifies helpful considerations that center patient comfort and quality of life during end-of-life care and can be applied to future cases navigating the transition of SMI patients to hospice care. Chochinov, H. M., Martens, P. J., Prior, H. J., & Kredentser, M. S. (2012). Comparative health care use patterns of people with schizophrenia near the end of life: a population-based study in Manitoba, Canada. Schizophrenia research, 141(2-3), 241-246.
Case:
Discussion:
Conclusion:
References:
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: Patients with serious mental illness face significant barriers in access to end-of-life services. Data shows that patients with SMI are less likely to be referred to and participate in end-of-life treatment, and hospice settings are often uncomfortable with managing patients with SMI. Within the SMI population, patients of color face an additional layer of stigma and barriers to care. While this submission considers ways to ease the transition of SMI patients to hospice care settings, further investigation is needed to determine how to best meet the needs of patients with both SMI and other marginalized identities in hospice care.

