Diversity, Equity, and Inclusion
(074) Potential Role of Bias in a Missed Neuropsychiatric Diagnosis in the Emergency Department: A Case Report and Literature Review

Reile M. Slattery, MD (she/her/hers)
CL Psychiatry Fellow
New York University Langone Health
New York, New York
Rebecca Breheney, MD (she/her/hers)
Resident in General Psychiatry and Professional Associate
New York-Presbyterian / Weill Cornell Medicine
New York, New York
Evguenia Makovkina, MD
Resident Physician
NewYork-Presbyterian Hospital/Weill Cornell Medicine
New York, New York
Justin Chen, MD, MPH
Vice Chair of Ambulatory Services & Vice Chair of Health Justice
Weill Cornell Medicine
New York, New York
Co-Author(s)
Presenting Author(s)
Co-Author(s)
Background: Neuropsychiatric symptoms are a common presenting complaint in the emergency department (ED). Misattribution of neuropsychiatric symptoms to primary psychiatric disorders leads to confusion amongst teams and families and prolonged suffering for patients. Here we report the case of a patient with catatonia to discuss the potential role of bias in missed organic etiologies of neuropsychiatric symptoms.
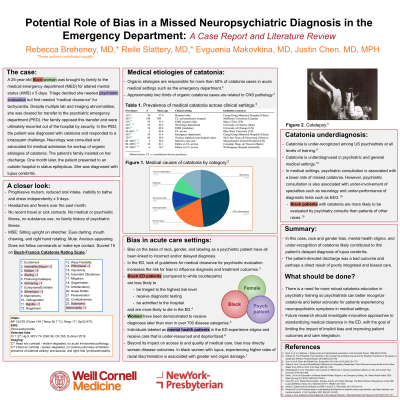
Case: A 25-year-old Black woman with no medical or psychiatric history presented to the ED with one week of disorganized behavior and mutism. Triage documented the chief complaint as “psychiatric evaluation,” though the patient and her family objected to involvement from psychiatry. She was persistently tachycardic with multiple lab abnormalities but was medically cleared for transfer to psychiatry without further workup. The patient’s family objected to the transfer, and communication rapidly devolved. Even though the ultimate recommendation was for a medical admission, the family no longer trusted the hospital to provide integrated multidisciplinary care, and the patient left against medical advice (AMA). On presentation to a different hospital one month later, the patient experienced a witnessed seizure and was diagnosed with lupus cerebritis.
Discussion: Bias on the basis of race, gender, and labeling as a psychiatric patient have all been linked to incorrect and/or delayed diagnosis. In the ED, a setting where there are no accepted guidelines for medical clearance for psychiatric evaluation (Tucci, 2015), biased care is particularly problematic. Black patients with catatonia are more likely to be evaluated by psychiatry consults than patients of other races (Llesuy, 2018), even though organic etiologies are responsible for more than 50% of catatonia in acute medical settings (Oldham, 2018). Women have been demonstrated to receive diagnoses later than men in over 700 disease categories (Westergaard, 2019). Individuals labeled as mental health patients in the ED experience stigma and receive care that is under-resourced and deprioritized (Smith, 2024).
Conclusion: In this case, bias and missed diagnosis in the ED may have led to a misattribution of catatonic symptoms to a primary psychiatric etiology. The patient’s AMA discharge was a bad outcome and perhaps a direct result of poorly integrated and biased care. Consult-liaison psychiatrists should be aware of these potential pitfalls to better advocate for patients experiencing neuropsychiatric symptoms in medical settings. Future research should investigate innovative approaches to standardizing medical clearance in the ED, aiming to improve patient outcomes and care integration.
References:
1) Tucci V, et al: Down the Rabbit Hole. Emerg Med Clin N Am 2015;33(4):721–737.
2) Llesuy J, et al: Catatonia Under-Diagnosis in the General Hospital. J Neuropsychiatry Clin Neurosci 2018;30(2):145–151.
3) Oldham M: The Probability That Catatonia in the Hospital has a Medical Cause and the Relative Proportions of Its Causes: A Systematic Review. Psychosomatics 2018;59(4):333–340.
4) Westergaard D, et al: Population-wide analysis of differences in disease progression patterns in men and women. Nat Commun 2019;10(1):666.
5) Smith J, et al: An Exploration of Mental Health-Related Stigma in an Emergency Setting. Int J Ment Health Addict 2024. https://doi.org/10.1007/s11469-023-01233-5.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: The subject of our case report, a young Black woman, represents an intersectional identity that is historically marginalized. We explore the impact of discrimination on her care in the emergency department and conclude that bias likely contributed to the misattribution of her neuropsychiatric symptoms to a primary psychiatric disorder. Our author group represents diversity of thought and expertise: two PGY4 psychiatry residents going into consult-liaison and addiction fellowships and one PGY3 resident considering a career in quality improvement led by a health justice expert. Furthermore, we bring varying cultural and ethnic backgrounds to our consideration of this case.

