Obesity, Nutrition, and Eating Disorders
(112) Post-Bariatric Avoidant/Restrictive Food Intake Disorder: A Case Report and Review of the Literature
- NC
Nadia Cacodcar, MD (she/her/hers)
C-L Fellow
Brigham and Women's Hospital
Boston, Massachusetts 
Shixie Jiang, M.D.
Assistant Professor
University of Florida College of Medicine
Gainesville, Florida
Presenting Author(s)
Co-Author(s)
Background:
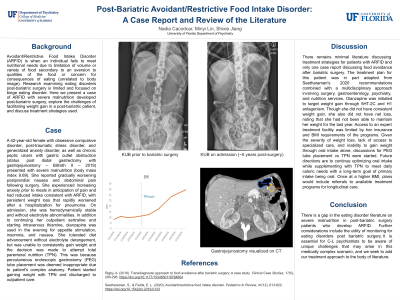
Avoidant/Restrictive Food Intake Disorder is when an individual fails to meet nutritional needs due to limitation of volume or variety of food secondary to an aversion to qualities of the food or concern for consequences of eating (unrelated to body image). Research examining eating disorders post-bariatric surgery is limited and focused on binge eating disorder. Here we present a case of ARFID with severe malnutrition developed post-bariatric surgery, explore the challenge of facilitating weight gain in a post-bariatric patient, and discuss treatment strategies used. A 42-year-old female with obsessive compulsive disorder, post-traumatic stress disorder, and generalized anxiety disorder, as well as chronic peptic ulcers with gastric outlet obstruction (status post distal gastrectomy with gastrojejunostomy Billroth II 2019) presented with severe malnutrition (body mass index 9.69). She reported gradually worsening postprandial nausea and abdominal pain following surgery. She experienced increasing anxiety prior to meals in anticipation of pain and reported reduced intake consistent with ARFID, having persistent weight loss that rapidly worsened after a hospitalization for pneumonia. On admission, she was hemodynamically stable and without electrolyte abnormalities. In addition to continuing her outpatient sertraline and starting intravenous thiamine, olanzapine was used in the evening for appetite stimulation, insomnia, and nausea. She tolerated diet advancement without electrolyte derangement, but was unable to consistently gain weight and the decision was made to place a percutaneous endoscopic gastrostomy (PEG) tube. There remains minimal literature discussing treatment strategies for patients with ARFID and only one case report discussing food avoidance after bariatric surgery. The treatment plan for this patient was in part adapted from Seetharaman’s 2020 recommendations combined with a multidisciplinary approach involving surgery, gastroenterology, psychiatry, and nutrition services. Olanzapine was initiated to target weight gain through 5HT2C and H1 antagonism. Though she did not have consistent weight gain, she also did not have net loss, noting that she had not been able to maintain her weight for the last year. Access to an expert treatment facility was limited by her insurance and BMI requirements of the programs. Given the severity of weight loss, lack of access to specialized care, and inability to gain weight through oral intake alone, discussions for PEG tube placement were started. Future directions are to continue optimizing oral intake while supplementing with tube feeds to meet daily caloric needs with a long-term goal of primary intake being oral. Once at a higher BMI, plans would include referrals to available treatment facilities for longitudinal care. There is a gap in the eating disorder literature on severe malnutrition in post-bariatric surgery patients who develop ARFID. It is essential for C-L psychiatrists to be aware of unique challenges that may arise in this medically complex scenario and we seek to add our treatment approach to the body of literature. Rigby, A. (2018). Transdiagnostic approach to food avoidance after bariatric surgery: A case study. Clinical Case Studies, 17(5), 280–295. https://doi.org/10.1177/1534650118784664
Case:
Discussion:
Conclusion:
References:
Seetharaman, S., & Fields, E. L. (2020). Avoidant/restrictive food intake disorder. Pediatrics In Review, 41(12), 613–622. https://doi.org/10.1542/pir.2019-0133
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: There is a need for more research looking at the risk of developing an eating disorder post-bariatric surgery in marginalized groups and how social and structural determinants impact this.

