Psycho-Oncology and Palliative Care
(121) Novel Use of Buprenorphine for Management of Pain in Hidradenitis Suppurativa
- JS
Jessica Schwartz, MD
Psychiatry Fellow
NYU Grossman School of Medicine
New York, New York - JS
Jessica Schwartz, MD
Psychiatry Fellow
NYU Grossman School of Medicine
New York, New York 
Soroush Pakniyat-Jahromi, MD
Fellow, Consultation-Liaison Psychiatry
NYU Langone Health
NY, New York
Soroush Pakniyat-Jahromi, MD
Fellow, Consultation-Liaison Psychiatry
NYU Langone Health
NY, New York- SS
Simon A. Sidelnik, MD
Director Addiction Consultation-Liaison Psychiatry
NYU Grossman School of Medicine
New York, New York - SS
Simon A. Sidelnik, MD
Director Addiction Consultation-Liaison Psychiatry
NYU Grossman School of Medicine
New York, New York 
Allison B. Deutch, MD
Program Director, Women's Mental Health Fellowship
NYU Langone Health, Manhattan Campus
New York, New York
Allison B. Deutch, MD
Program Director, Women's Mental Health Fellowship
NYU Langone Health, Manhattan Campus
New York, New York
Presenting Author(s)
Co-Author(s)
Background:
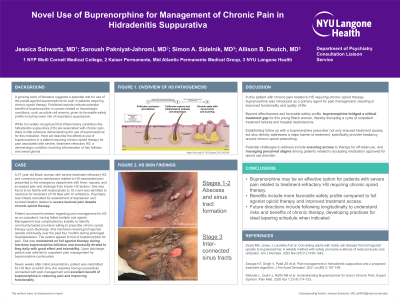
A growing body of literature outlines a role for use of buprenorphine for pain in patients requiring long-term opioid therapy. Published reports indicate potential benefit of buprenorphine in cancer-related or hematologic conditions such as sickle cell anemia given its favorable safety profile. While it is widely recognized that inflammatory conditions like hidradenitis suppurativa (HS) are associated with chronic pain, there is little evidence demonstrating the use of buprenorphine in these cases. Here we describe the effective use of buprenorphine in a patient requiring chronic opioid therapy for pain associated with severe, treatment refractory HS, a dermatologic condition involving inflammation of hair follicles and sweat glands.
Case:
A 27-year-old Black woman with treatment-refractory HS and prior admissions for intravenous pain control, presented to the emergency department with fever, nausea, and increased pain and drainage from known HS lesions. She was found to be febrile with leukocytosis to 19.3 and was admitted to medicine for treatment of HS flare with IV antibiotics. Psychiatry was initially consulted for assessment of depression and suicidal ideation related to severe lesional pain despite chronic opioid therapy.
Patient conveyed frustration regarding pain management for HS as an outpatient, having failed multiple oral agents. Management was further complicated by inability to identify community-based providers willing to prescribe chronic opioid therapy upon discharge. Patient agreed to trial of buprenorphine for pain. She was maintained on full agonist therapy during low-dose buprenorphine microinduction, and eventually titrated to 6mg daily with good effect and tolerability. Upon discharge, patient was referred to outpatient pain management for buprenorphine continuation.
Seven weeks after initial presentation, she was readmitted for HS flare at which time she reported having successfully connected with pain management and excellent benefit of buprenorphine in reducing pain and improving functionality.
Discussion:
In this patient with chronic pain related to HS requiring long-term opioid therapy, buprenorphine was introduced as a primary agent for pain management, resulting in improved functionality and quality of life. Beyond effectiveness and safety, buprenorphine bridged a critical treatment gap for this young Black woman, thereby disrupting a vicious cycle of outpatient treatment failures and hospital readmissions. Establishing follow up with a buprenorphine prescriber not only ensured treatment access, but also directly addressed a major barrier to treatment access, specifically provider hesitancy around chronic opioid prescribing.
Conclusion:
Buprenorphine may be an effective option for patients with severe pain related to treatment-refractory HS requiring chronic opioid therapy. Benefits include more favorable safety profile compared to full opioid agonist therapy and improved treatment access.
References:
David MS, Jones J, Lauriello A et al. Converting adults with sickle cell disease from full agonist opioids to buprenorphine: A reliable method with safety and early evidence of reduced acute care utilization. Am J Hematol. 2022 Nov;97(11):1435-1442.
Savage KT, Singh V, Patel ZS et al. Pain management in hidradenitis suppurativa and a proposed treatment algorithm. J Am Acad Dermatol. 2021 Jul;85(1):187-199.
Webster L, Gudin J, Raffa RB et al. Understanding Buprenorphine for Use in Chronic Pain: Expert Opinion. Pain Med. 2020 Apr 1;21(4):714-723.
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: Racial and ethnic disparities in treatment for pain are widely recognized. Black, Indigenous, and Other People of Color (BIOPC) patients are too often subject to biases and stigma on the part of healthcare providers and systems, limiting access to adequate pain management. In this case, we illustrate that transition to use of buprenorphine for pain management in a young black woman not only provided more reliable access to specialized care for pain, but also helped to legitimize need for ongoing pain management for hidradenitis supppurativa, and interrupted a pattern of repeated inpatient admissions for intravenous pain control.

