Catatonia
(028) NMS-induced PRES with resultant catatonia successfully treated by ECT

J. Cody Naughton, MD (he/him/his)
Fellow Psychiatrist
Brigham and Women's Hospital / Dana Farber Cancer Institute
Boston, Massachusetts- GK
Genevieve Kupsky, MD
Resident Physician
Rush University Medical Center
Chicago, Illinois 
Aniruddha Deka, MD (he/him/his)
Assistant Professor of Psychiatry & Behavioral Sciences; Medical Director of Transplant Psychiatry
Rush University Medical Center
Chicago, Illinois
Presenting Author(s)
Co-Author(s)
Background
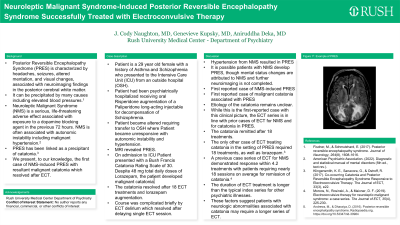
Posterior Reversible Encephalopathy Syndrome (PRES) is characterized by headaches, seizures, altered mentation, visual changes, and is associated with neuroimaging findings in the posterior cerebral white matter. One precipitant can be hypertension (Fischer, 2017). Neuroleptic Malignant Syndrome (NMS) is a life-threatening adverse effect associated with exposure to a dopamine blocking agent. NMS is associated with autonomic instability including malignant hypertension (American Psychiatric Association, 2022). We present a case of NMS-induced PRES with resultant malignant catatonia which resolved after ECT. To our knowledge it is the first case to describe PRES associated with NMS.
Case RM is a 29 year old female with a history of Asthma and Schizophrenia who presented to the Intensive Care Unit (ICU) from an outside hospital (OSH). RM had been psychiatrically hospitalized receiving oral antipsychotic augmentation of a long-acting injectable for decompensation of Schizophrenia. RM became altered requiring transfer to OSH where RM became unresponsive with autonomic instability and hypertension. MRI revealed PRES. On admission to ICU RM presented with a Bush Francis Catatonia Rating Scale of 30. Despite high total daily doses of Lorazepam, the patient developed malignant catatonia. The catatonia resolved after 18 ECT treatments and lorazepam augmentation. Discussion In this case, the hypertension from NMS resulted in PRES. Given comorbid PRES and NMS, the precise etiology of the catatonia remains unclear.This case highlights the importance of early recognition and treatment of NMS. It is possible patients with NMS develop PRES, though mental status changes are attributed to NMS and further neuroimaging is not completed. This case is important as it is the first reported case of NMS-induced PRES. It is also the first reported case of malignant catatonia associated with PRES. Finally, the ECT series for RM is in line with prior cases of ECT for NMS and for catatonia in PRES. RM achieved remission of catatonia after 18 treatments. The only other case of ECT treating catatonia in the setting of PRES required 18 treatments, as well as lorazepam (Klingensmith. 2017).A previous case series of ECT for NMS demonstrated response within 4.2 treatments with patients requiring nearly 18 sessions on average for remission of catatonia (Morcos, 2019). Notably, the duration of ECT treatment is longer than the typical index series for other psychiatric illnesses. These factors suggest patients with neurologic abnormalities associated with catatonia may require a longer series of ECT. Conclusion Vigilant monitoring for emergence of PRES may be warranted in patients with NMS. ECT can be a safe and effective treatment for these rare neuropsychiatric complications. References American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (5th ed., text rev.). Fischer, M., & Schmutzhard, E. (2017). Posterior reversible encephalopathy syndrome. Journal of Neurology, 264(8), 1608-1616. Klingensmith, K. E., Sanacora, G., & Ostroff, R. (2017). Co-occurring Catatonia and Posterior Reversible Encephalopathy Syndrome Responsive to Electroconvulsive Therapy. The Journal of ECT, 33(3), e22.
Morcos, N., Rosinski, A., & Maixner, D. F. (2019). Electroconvulsive therapy for neuroleptic malignant syndrome: a case series. The Journal of ECT, 35(4), 225-230.
Presentation Eligibility: No plans for publication prior to November 2024
Diversity, Equity, and Inclusion: This case is one focused on a patient from a historically marginalized patient population. The patient is part of a population in which symptoms historically have been under-treated compared to other populations. The three co-authors are a selection of individuals from diverse backgrounds and a diverse range of clinical training and experience.

