Neurocognitive Disorders and Neuropsychiatry
(096) Navigating Medical Mistrust in Consultation-Liaison Psychiatry - Case Report and Literature Review of Ivermectin-Induced Cognitive Impairment

Alexander Swartz, DO (he/him/his)
PGY-2, Psychiatry
Rowan-Virtua School of Osteopathic Medicine Department of Psychiatry
Voorhees Township, New Jersey
Daniel Somma, Doctor of Osteopathic Medicine (DO)
Psychiatry Resident
Rowan-Virtua School of Osteopathic Medicine Department of Psychiatry
Cherry Hill, New Jersey.jpg)
Timothy L. Wong, DO
Director of Consultation-Liaison Psychiatry, Associate Program Director of Residency Training
Rowan-Virtua School of Osteopathic Medicine
Philadelphia, Pennsylvania
Presenting Author(s)
Co-Author(s)
Background
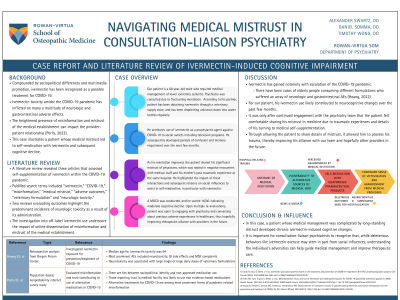
Ivermectin toxicity amidst the COVID-19 pandemic has inflicted on many a multitude of neurologic and gastrointestinal adverse effects. The heightened presence of misinformation and mistrust of the medical establishment can impact the provider-patient relationship (Perlis, 2023). This case illustrates a patient whose medical mistrust led to self-medication with ivermectin and subsequent cognitive decline.
Case
Our patient is a 68 year-old male who required medical management of lower extremity cellulitis. Psychiatry was consulted due to fluctuating mentation. According to his partner, patient has been obtaining ivermectin through a veterinary supply store, and has been dropletting unknown doses into water bottles regularly. He attributes use of ivermectin as a prophylactic agent against COVID-19 to social outlets including television programs. He subsequently developed periods of confusion and memory impairment over the next few months.
As his mentation improved, the patient shared his significant mistrust of physicians, which was rooted in negative encounters with medical staff and his mother’s past traumatic experience at the same hospital. He highlighted the impact of these interactions and subsequent reliance on social influences to assist in self-medication, in particular with ivermectin. A MOCA was conducted, and he scored 16/30 indicating moderate cognitive decline.
Literature Review
A literature review revealed three articles that assessed self-supplementation of ivermectin within the COVID-19 pandemic. Two reviews evaluating outcomes highlight the predominant incidence of neurologic toxicity as a result of its administration. The investigation into off-label ivermectin use underscore the impact of online dissemination of misinformation and mistrust of the medical establishment.
Discussion
Ivermectin has gained notoriety with escalation of the COVID-19 pandemic. There have been cases of elderly people consuming different formulations who suffered an array of neurologic and gastrointestinal AEs (Hoang, 2022). For our patient, his ivermectin use likely contributed to neurocognitive changes over the past few months. It was only after continued engagement with the psychiatry team that the patient felt comfortable sharing his mistrust in medicine due to traumatic experiences and details of his turning to medical self-supplementation. Through allowing the patient to share details of mistrust, it allowed him to process his trauma, thereby improving his alliance with our team and hopefully other providers in the future.
Conclusions/Influence
In this case, a patient whose medical management was complicated by long-standing distrust developed chronic ivermectin-induced cognitive changes. It is important for consultation-liaison psychiatrists to recognize that, while deleterious behaviors like ivermectin overuse may stem in part from social influences, understanding the individual’s adversities can help guide medical management and improve therapeutic care.
References
Perlis RH, Lunz Trujillo K, Green J, et al. Misinformation, Trust, and Use of Ivermectin and Hydroxychloroquine for COVID-19 [published correction appears in JAMA Health Forum. 2023 Oct 6;4(10):e234083]. JAMA Health Forum. 2023;4(9):e233257. Published 2023 Sep 1. doi:10.1001/jamahealthforum.2023.3257
Hoang R, Temple C, Correia MS, Clemons J, Hendrickson RG. Characteristics of ivermectin toxicity in patients taking veterinary and human formulations for the prevention and treatment of COVID-19. Clin Toxicol (Phila). 2022;60(12):1350-1355. doi:10.1080/15563650.2022.2134788
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: This case report highlights the unique role of consultation-liaison psychiatry to maintain an inclusive environment, dissect trauma and accept sociopolitical diversity to enhance the provider-patient relationship. The patient in our case faced significant stigmatization and trauma predominantly in the medical setting, and as a result, turned to political outlets for health-related information. Current political climate demands a fine balance between sociopolitical viewpoints and the fragile trust of the medical establishment. Thus, there was a requirement to not only manage countertransference, but to also understand the patient’s perspective in order to maintain an inclusive therapeutic environment and provide equitable care.

