Quality and Safety
(162) From Consultant to Consultee: Lessons from a Medical Psychiatry Unit

Ariel Shalev, MD (she/her/hers)
Resident
Weill Cornell Medicine
New York, New York- ML
Michael Liu, n/a
Medical Student
Weill Cornell Medicine
New York, New York 
Daniel Shalev, MD (he/him/his)
Assistant Professor
Weill Cornell Medicine
New York, New York
Presenting Author(s)
Co-Author(s)
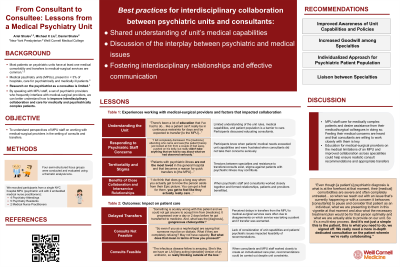
Background/Significance: Patients admitted to inpatient psychiatry units frequently have acute medical comorbidities and require non-psychiatric care (Lyketsos, 2002). For inpatient psychiatric unit staff, this means interfacing with non-psychiatric specialists to coordinate consults, transfers, and follow-up care. Existing literature examines the role of psychiatrists as consultants, yet research into the psychiatrist as a consultee is limited. Existing literature suggests that this relationship can be complex and that consultants may experience discomfort on the psychiatric unit (Bernstein, 1980). To address this gap we set out to characterize the inpatient psychiatric staff experience of working with non-psychiatric providers in the setting of transfers and consults using qualitative methods. Lack of clarity regarding the unit’s medical limitations among non-psychiatric providers is an obstacle to providing timely and appropriate medical care. When non-psychiatric providers consider a patient’s psychiatric illness and psychosocial circumstances while providing medical care, effective care plans can be made. Close collaboration between psychiatric and non-psychiatric providers when providing medical care is crucial, as psychiatric teams can leverage patient trust and rapport to improve consultants’ ability to provide care. Lyketsos CG, Dunn G, Kaminsky MJ, Breakey WR. Medical comorbidity in psychiatric inpatients: relation to clinical outcomes and hospital length of stay. Psychosomatics. 2002;43(1):24-30. doi:10.1176/appi.psy.43.1.24
Methods: We conducted a quality improvement study utilizing small (two to four participant), semi-structured focus groups with clinical staff from Weill Cornell’s medical psychiatry unit (MPU; an inpatient psychiatric unit able to accommodate patients with medical comorbidities). Inclusion criteria included MPU clinical staff (psychiatry residents and attendings, and medical nurse practitioners working on the psychiatric unit) involved in at least one consult or transfer for an MPU patient. Qualitative data was recorded, transcribed, and coded using an iterative inductive-deductive thematic analysis approach. IRB approval was received.
Results: Two out of six (one embedded medical nurse practitioner group, two attending psychiatry groups, three resident psychiatry groups) small (two to four participant), semi-structured focus groups have been conducted thus far. Three key themes emerged from our data:
Discussion: Psychiatric staff play a key role in ensuring that non-psychiatric specialists are equipped to care for psychiatric inpatients. There has been limited exploration of the practice of psychiatry consultee-liaisons (Bernstein, 1990). Although our findings are drawn from a single unit at this stage in our study, they serve as important, hypothesis-generating work to improve consultee-liaisonship.
Conclusion/Implications: Our qualitative, exploratory study provides a preliminary framework to consider best practices for psychiatric consultees. Actionable tools include the importance of educating consultants on the limitations of the psychiatric unit, serving as a bridge between non-psychiatric providers and patients, and ensuring that care plans are realistic and feasible in the context of a patient’s psychiatric illness.
References:
Bernstein RA. Liaison psychiatry: a model for medical care on a general hospital psychiatric unit. Gen Hosp Psychiatry. 1980;2(2):141-147. doi:10.1016/0163-8343(80)90028-6
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: People with severe mental illness have historically had poorer access to medical care and worse medical outcomes. These disparities are partly due to the siloing of medical and psychiatric care and stigma among non-psychiatric clinicians. By better understanding obstacles between collaborating psychiatric and non-psychiatric clinicians, we can create strategies to promote effective interdisciplinary care for patients with both medical and psychiatric needs.

