Neurocognitive Disorders and Neuropsychiatry
(090) Familial Hemiplegic Migraine and Psychosis
- AK
Alison Kor, MD (she/her/hers)
Psychiatry Resident
Mayo Clinic
Rochester, Minnesota - VD
Vanessa Dang, MD (she/her/hers)
Psychiatrist
Mayo Clinic - Rochester
Rochester, Minnesota - JP
Judit Perez Ortiz, MD, PhD
Child and Adolescent Neurology Resident
Mayo Clinic
Rochester, Minnesota - CS
Christopher Sola, DO, FACLP
Psychiatrist
Mayo Clinic
ROCHESTER, Minnesota
Presenting Author(s)
Co-Author(s)
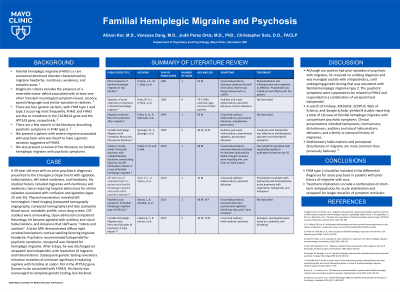
Background/Significance: Familial hemiplegic migraine (FHM) is a rare autosomal dominant disorder characterized by migraine headache, numbness, weakness, and complex auras (Maksemous, 2019). A few reports in the literature describe psychotic symptoms in FHM type 2. We present a patient with severe migraine associated with psychosis who was found to have a genetic variation suggestive of FHM2. We also present a review of the literature on familial hemiplegic migraine with psychotic symptoms.
Case: A 49-year-old man with no prior psychiatric diagnoses presented to the Emergency Department with agitation, hallucinations, left-sided numbness, and headache. His medical history included migraines with numbness and weakness, twice requiring hospital admissions for similar episodes associated with confusion and agitation (ages 25 and 35). Physical examination revealed left hemineglect. Head imaging (computed tomography angiography, computed tomography) and labs (complete blood count, metabolic profile, urine drug screen, CSF studies) were unrevealing. Upon admission to inpatient Neurology, he became agitated with auditory and visual hallucinations, and delusions that staff were “robots and zombies”. A brain MRI demonstrated diffuse right cerebral hemispheric cortical swelling favoring migraine headache. Psychiatry recommended haloperidol for psychotic symptoms. Verapamil was initiated for hemiplegic migraine. After 6 days, he was discharged on verapamil and haloperidol, with resolution of migraine and hallucinations. Subsequent genetic testing revealed a missense mutation of unknown significance replacing arginine with histidine at codon 763 in the ATP1A2 gene (known to be associated with FHM2). His family was encouraged to complete genetic testing but declined.
Discussion: Although our patient had prior episodes of psychosis with migraine, he received no unifying diagnosis and was managed acutely with antipsychotics, until undergoing genetic testing that was consistent with familial hemiplegic migraine type 2. The psychotic symptoms were suspected to be related to FHM2 and responded to a combination of verapamil and haloperidol. A search of Embase, MEDLINE, SCOPUS, Web of Science, and Google Scholar yielded 8 studies reporting a total of 18 cases of familial hemiplegic migraine with concomitant psychotic symptoms. Clinical presentations included hemiparesis, hemisensory disturbances, auditory and visual hallucinations, delusions, and a family or personal history of migraines. Multisensory hallucinations and perceptual disturbances in migraine are more common than previously believed (Li, 2024).
Conclusions/Implications: FHM type 2 should be included in the differential diagnoses for acute psychosis in patients with prior history of migraine with aura. Treatment implications include a combination of short-term antipsychotics for acute stabilization and verapamil for longer duration of symptom remission.
References:
Li Y, Yolland COB, et al.: Multisensory hallucinations and other unusual sensory experiences in the context of migraine: a systematic review. Journal of Neurology 2024; 271: 1717-1746.
Maksemous N, Smith RA, et al.: Targeted next generation sequencing identifies a genetic spectrum of DNA variants in patients with hemiplegic migraine. Cephalalgia Reports 2019; 2: (no pagination).
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: Familial hemiplegic migraine is rare but has serious implications for affected patients. Our poster highlights important considerations related to psychosis identification and treatment. This relates to ensuring equity in care for all patients, especially related to a rare disease.

