Quality and Safety
(161) Establishing Best Practice Benchmarks in Emergency Psychiatry: A National Survey
.jpg)
Julie R. Owen, MD, FAPA (she/her/hers)
Assistant Professor
Medical College of Wisconsin
Milwaukee, Wisconsin
Kahaan Patel, MD
Medical Resident
MCWAH
Brookfield, Wisconsin
Presenting Author(s)
Co-Author(s)
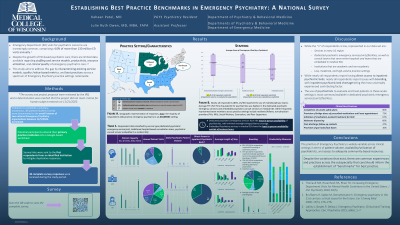
Background/Significance: Emergency Department (ED) visits for psychiatric concerns are increasingly common, comprising >10% of more than 130 million ED visits annually (Theriault, 2020). Despite the growth of ED-based psychiatric care, there are limited data available regarding staffing and service models, productivity, resource utilization, and clinical quality of emergency psychiatric care (Bruffaerts, 2008; Lofchy, 2015). This study aims to address this gap by characterizing existing service models, quality-/value-based metrics, and best practices across a spectrum of Emergency Psychiatry practice settings nationwide.
Methods: Invitations to complete a voluntary, anonymous, 30-question Qualtrics survey were disseminated to the email listservs of two national Emergency Psychiatry organizations between 12/5/2023-2/23/2024. Potential participants entered their primary practice institution into a Google-based worksheet, and survey links were sent to the first respondents from an identified institution to mitigate duplicative responses. 30 complete survey responses were received. The survey and project proposal were reviewed by the IRB, and a determination was reached that the project did not meet criteria for human subject research on 11/21/2023.
Results: 30 respondents representing all geographic regions of the United States reported on coverage hours by psychiatrists (averaging 24-35 hours per week), accessibility and delivery of services across different shifts (with in-person services predominant, particularly during business hours), and annual ED patient volumes (ranging from < 10,000 to >100,000 annual visits). Over 70% of respondents reported having access to inpatient psychiatric units. Frequent ED boarding of psychiatric patients was observed in approximately 60% of settings, with identified causes including community inpatient psychiatric bed shortages and transportation issues. Most respondents expressed uncertainty or dissatisfaction with the adequacy of training for emergency medicine (EM) physicians and trainees in managing acute psychiatric presentations; some institutions offered psychiatry-specific EM training. Quality metrics were commonly utilized to measure service performance and value, with metrics including service response time, restraint use, ED readmissions, and length of stay. Clinical best practices included initiation of medication-assisted treatment for substance use disorders, completion of suicide safety plans, provision of bridge psychotropic medication prescriptions, and naloxone dispensing.
Discussion: While Emergency Psychiatry is practiced using diverse models of service delivery and staffing, there are common practices and challenges across settings and geographic regions. These data can be utilized to drive practice benchmarks and best practice guidelines for a growing subspecialty.
Conclusions/implications: Data collected from emergency psychiatrists practicing in a variety of service delivery models from every region of the United States can contribute to a better understanding of the current landscape of emergency psychiatric care and can inform efforts to enhance the quality and effectiveness of services in this critical area of healthcare.
References:
Bruffaerts R, Sabbe M, Demyttenaere K. Emergency psychiatry in the 21st century: critical issues for the future. Eur J Emerg Med 2008; 15(5), 276–278. https://doi.org/10.1097/MEJ.0b013e3282fc7616
Lofchy J, Boyles P, Delwo J. Emergency Psychiatry: Clinical and Training Approaches. Can J Psychiatry 2015; 60(6), 1–7.
Theriault KM, Rosenheck RA, Rhee TG: Increasing Emergency Department Visits for Mental Health Conditions in the United States. J Clin Psychiatry 2020; 81(5).
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: Emergency psychiatry services serve as a lens to examine disparities in mental healthcare access. By exploring factors influencing service utilization among diverse populations, including minorities and LGBTQ+ individuals, we unveil systemic barriers. Understanding this interplay informs targeted interventions, promoting equity. Culturally competent care advocacy within emergency psychiatry fosters inclusivity, addressing marginalized communities' unique needs and advancing diversity in medicine.

