Quality and Safety
(160) Enhancing Decision-Making Capacity Assessment in Inpatient Care Teams: A Quality Improvement Project at Lehigh Valley Health Network

Rachael J. Murphy, MD
Resident Physician
Lehigh Valley Health Network
Bethlehem, Pennsylvania
Presenting Author(s)
Background/Significance: Assessing decision-making capacity (DMC) is critical in clinical practice, yet challenges persist in effectively conducting these assessments. This project aimed to evaluate the impact of an educational program on DMC for LVHN inpatient care teams consulting the Psychiatry C/L Service. Given the complexity of DMC assessments and the involvement of multiple team members, there is a need to enhance education and streamline processes to ensure comprehensive and efficient evaluations.
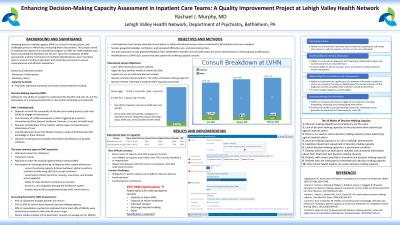
Methods: A retrospective chart review assessed consult patterns, while educational sessions were conducted for IM residents and case managers. Surveys gauged knowledge, confidence, and perceived difficulties pre- and post-intervention. Proposed modifications to LVHN's Epic system included options for ordering capacity consults: capacity to leave AMA, capacity to refuse treatment, informed consent, discharge decision-making, or other. The post-education survey gathered feedback from LVHN staff to identify common difficulties and assess receptiveness to the proposed modifications.
Results: The educational program led to improved knowledge and confidence levels among participants. Pre-education quiz results showed that residents had a mean total correct score of 73% (with the lowest score at 33% and the highest at 93%), while case workers had a mean total correct score of 73% (with the lowest at 47% and the highest at 87%). Common difficulties identified included ambiguities in patient capacity across different decision domains, challenges related to family dynamics, and interdisciplinary coordination. Post-education survey data revealed that most respondents expressed support for the proposed Epic modifications, with 94% of residents and 96% of caseworkers agreeing that a specifier in the Epic order to consult Psychiatry C/L would improve efficiency during capacity assessments. These changes were subsequently implemented and have received positive feedback, enhancing communication and efficiency in capacity assessments thus far.
Discussion: This project underscores the importance of targeted education and system enhancements in optimizing DMC assessments. Addressing challenges such as defining specific assessment questions and improving interdisciplinary collaboration can contribute to more accurate and streamlined evaluations. The successful implementation of the proposed Epic modifications demonstrates their potential to standardize and improve the efficiency of capacity consultations.
Conclusion/Implications: Addressing knowledge gaps and clarifying capacity assessment processes with an educational program has improved the quality of DMC assessments within LVHN's inpatient settings. The implementation of streamlined ordering options in the EMR as demonstrated in this project has the potential to significantly enhance communication, efficiency, and ultimately, patient care within other healthcare settings as well.
References:
Appelbaum PS, Assessment of Patients’ Competence to Consent to Treatment, JAMA 2007;357(18):1834-1840.
Charles L, Parmar J, Brémault-Phillips S, Dobbs B, Sacrey L, Sluggett B. Physician education on decision-making capacity assessment: Current state and future directions. Can Fam Physician. 2017;63(1):e21-e30.
Ganzini L, Volicer L, Nelson WA, Fox E, Derse AR. Ten myths about decision-making capacity. J Am Med Dir Assoc. 2004;5(4):263-267.
Lamont S, Jeon Y, Chiarella M. Health-care professionals’ knowledge, attitudes and behaviours relating to patient capacity to consent to treatment: An integrative review. Nursing Ethics. 2013;20(6):684-607.
Seyfried L, Ryan KA, Kim SY. Assessment of decision-making capacity: views and experiences of consultation psychiatrists. Psychosomatics. 2013;54(2):115-23.
Presentation Eligibility: Not previously published or presented
Diversity, Equity, and Inclusion: This project enhances DEI by advocating for culturally sensitive decision-making capacity assessments, considering the unique challenges faced by historically marginalized groups. It aims to mitigate disparities by addressing barriers to understanding and accessing healthcare, particularly for individuals with limited English proficiency, varying cultural beliefs, or socioeconomic challenges. By promoting education and system improvements, it strives to ensure equitable treatment and respect for diverse perspectives. Ultimately, integrating DEI principles into capacity evaluations will empower marginalized individuals, enhancing their autonomy and fostering trust in the healthcare system.

