Transplant Psychiatry and C-L Subspecialties
(211) Enhanced Screening for ADHD in Patients with Alcohol Use Disorder and Alcohol-Associated Liver Disease: A Retrospective Cohort Study Assessing Preventive Potential in Liver Transplantation

Alexis L. Carnduff, MD (she/her/hers)
Resident Physician
University of Washington
Seattle, Washington
Ana Ivkovic, MD, FACLP
Staff Psychiatrist, Massachusetts General Hospital; Assistant Professor, Harvard Medical School
Massachusetts General Hospital
Boston, Massachusetts
Kelly C. Hsu, BS
Medical Student
Tufts University School of Medicine
Boston, Massachusetts- WZ
Wei Zhang, MD PhD
Assistant Professor
Massachusetts General Hospital
BOSTON, Massachusetts
Presenting Author(s)
Co-Author(s)
Background/Significance:
Attention Deficit Hyperactivity Disorder (ADHD) is a recognized risk factor for developing substance use disorders, including Alcohol Use Disorder (AUD). Moreover, treatment of ADHD appears to improve AUD outcomes. Despite this, screening for ADHD is not protocolized in AUD treatment guidelines, and ADHD remains under-recognized and undertreated in individuals with addiction. This underrecognition may inadvertently contribute to the global burden of AUD-related morbidity, including alcohol-associated liver disease (ALD), which is currently the leading indication for liver transplantation worldwide. This study aims to assess childhood-onset ADHD prevalence in ALD patients post-OLT and emphasize early intervention in high-risk groups.
Methods:
We conducted a retrospective cohort study at Massachusetts General Hospital's Long-term Individualized Follow-up after Transplant (LIFT) Clinic, focusing on ALD patients who received OLT from 2016 to 2023. Patient data, including ADHD prevalence, were gathered from electronic medical records. ADHD screening, including clinical interview and the Adult ADHD Self-Report Scale (ASRS), was routinely implemented in post-transplant follow-up. To address cognitive impairment from liver disease, we ensured positive screenings reflected symptoms from childhood or adolescence. Ethical guidelines were strictly followed.
Results
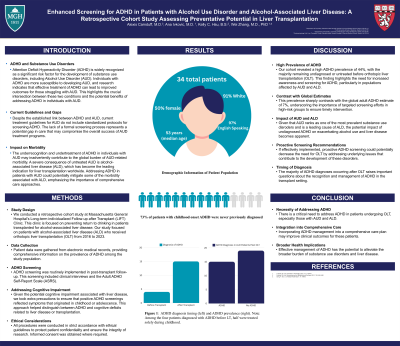
A total of 34 patients were included, with a median age of 53 years. Half the cohort (n=17) was female. Most patients identified as White (91%, n=31) and English-speaking (97%, n=33). A significant minority (44% (n=15) of the total cohort) was diagnosed with ADHD, with only 26% (n=4) of these patients diagnosed before liver transplantation. Notably, 73% (n=11) of the patients with childhood-onset ADHD were never previously diagnosed and only received the diagnosis because of routine screening in our post-LT clinic. Moreover, among the four patients diagnosed with ADHD before LT, half of them were treated solely during childhood. They did not continue treatment into adulthood, despite previous benefit from stimulant medication.
Discussion
Our cohort revealed a high ADHD prevalence (44%), with the majority remaining undiagnosed or untreated before OLT. This contrasts sharply with the global adult ADHD estimate (7%), underscoring the need for increased awareness and screening, particularly in populations with AUD and ALD. Given that AUD ranks as one of the most prevalent substance use disorders and is a leading cause of ALD, the potential impact of undiagnosed ADHD on exacerbating alcohol use and liver disease becomes apparent. This prompts consideration of whether proactive ADHD screening could have prevented or reduced AUD and ALD onset, potentially decreasing the need for OLT. Furthermore, the majority of ADHD diagnoses occurred after OLT, raising important questions about prompt ADHD recognition and management in the transplant setting. Conclusion Our study underscores the necessity of addressing ADHD in OLT patients, especially those with AUD and ALD. Integrating ADHD management into comprehensive care may improve outcomes and alleviate the burden of substance use and liver disease on a broader scale. References Luderer, M. et al. Frontiers in Psychiatry 2023; 14: 1112843. Luderer, M. et al. Neuroscience and Biobehavioral Reviews 2021; 128: 648–660. Song, P. et al. J of Global Health 2021; 11: 04009.
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: Our study highlights the prevalence of undiagnosed and untreated ADHD within a population often neglected and marginalized by the healthcare system—those with substance use disorders. Addiction affects individuals regardless of race, ethnicity, or socioeconomic status. Yet, our healthcare industry has historically overlooked the unique needs of these individuals, perpetuating inequities in access to diagnosis and treatment. Implementing protocolized screening for ADHD early post-transplantation is a step towards rectifying these disparities and helps ensure equitable, proactive, and evidence-based treatment for all individuals, regardless of their background or struggles with substance use disorders.

