Psychopharmacology and Toxicology
(139) Emerging Perspectives: GLP-1 Agonists and Lithium Toxicity - A Case Report

Ashley Kunnath, MD
General Psychiatry PGY3 Resident
Northwell Health
New Hyde Park, New York.jpg)
Jisha Lovin Kuriakose, MD
Attending Psychiatrist, Consultation Liaison Psychiatry
New Hyde Park
New Hyde Park, New York
Presenting Author(s)
Co-Author(s)
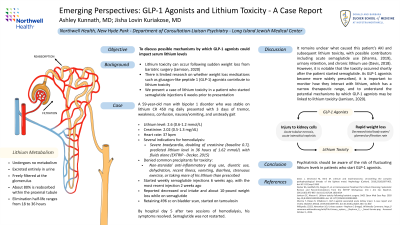
Background/Significance: Lithium toxicity has been documented to occur following sudden weight loss from bariatric surgery (Jamison, 2020). However, there is limited research on whether weight loss medications such as glucagon-like peptide 1 (GLP-1) agonists could contribute to lithium toxicity. We present a case of lithium toxicity in a patient who started semaglutide injections 6 weeks p</span>rior to presentation. Davis J, Desmond M, Berk M. Lithium and nephrotoxicity: Unravelling the complex pathophysiological threads of the lightest metal. Nephrology (Carlton). 2018;23(10):897-903. doi:10.1111/nep.13263 Decker BS, Goldfarb DS, Dargan PI, et al. Extracorporeal Treatment for Lithium Poisoning: Systematic Review and Recommendations from the EXTRIP Workgroup. Clin J Am Soc Nephrol. 2015;10(5):875-887. doi:10.2215/CJN.10021014 Jamison SC, Aheron K. Lithium toxicity following bariatric surgery. SAGE Open Med Case Rep. 2020 Sep 10;8:2050313X20953000. doi: 10.1177/2050313X20953000. PMID: 32974026; PMCID: PMC7491210. Sharma T, Paixao R, Villabona C. GLP-1 agonist associated acute kidney injury: A case report and review. Diabetes Metab. 2019;45(5):489-491. doi:10.1016/j.diabet.2017.12.002
Case: The patient is a 59-year-old man with a history of bipolar disorder who was stable on lithium CR 450 mg daily. He presented with 3 days of tremor, weakness, nausea/vomiting, and unsteady gait. He was found to have a lithium level of 2.6 (0.6-1.2 mmol/L), acute kidney injury (AKI) with creatinine of 2.02 (0.5-1.3 mg/dL), and heart rate of 37. There were several indications for hemodialysis including severe bradycardia, doubling of creatinine (baseline 0.7), and predicted lithium level in 36 hours of 1.62 mmol/L with fluids alone (Decker, 2015). He denied any precipitants for toxicity including non-steroidal anti-inflammatory drug (NSAID) use, diuretic use, dehydration, recent illness, vomiting, diarrhea, strenuous exercise, or taking more of his lithium than prescribed. However, he started weekly semaglutide injections 6 weeks ago, with the most recent injection 2 weeks prior to presentation. The p</span>atient did admit to decreased oral intake and weight loss while on semaglutide. During his hospital course, he was found to be retaining 496 cc of urine on bladder scan and was started on tamsulosin. By hospital day 5 after two sessions of hemodialysis, his symptoms resolved and his kidney function normalized.
Discussion: It remains unclear what caused this patient’s AKI and subsequent lithium toxicity, with possible contributors including acute semaglutide use (Sharma, 2019), urinary retention, and chronic lithium use (Davis, 2018). However, it is notable that the toxicity occurred shortly after the patient started semaglutide. As GLP-1 agonists become more widely prescribed, it is important to monitor how they interact with lithium, which has a narrow therapeutic range. There are multiple theoretical mechanisms by which semaglutide may be linked to lithium toxicity, ranging from direct injury to kidney cells (acute tubular necrosis, acute interstitial nephritis) to indirect effects of rapid weight loss on lithium elimination (decreased total body water, glomerular filtration rate, and renal blood flow) (Jamison, 2020). Psychiatrists should be aware of the risk of fluctuating lithium levels in patients who start GLP-1 agonists.
Conclusion: GLP-1 agonists may be associated with increased lithium levels through the mechanisms of AKI and rapid weight loss impacting pharmacokinetics.
References:
Presentation Eligibility: Not previously published or presented.
Diversity, Equity, and Inclusion: Although this topic does not relate directly to DEI, understanding any possible links between lithium toxicity and semaglutide could help us safely treat our psychiatric patients, who are often members of marginalized groups. As both authors are South Asian women, the submission would also work towards racial and gender-based parity in academic spaces.

