Psycho-Oncology and Palliative Care
(119) Effects of steroid exposure on neuropsychiatric events in cancer patients undergoing immune checkpoint inhibitors.

Deepti Chopra, MD, MPH
Associate Professor
MD Anderson Cancer Center
Houston, Texas- TL
Tamara Lacourt, PhD
Assistant Professor
MD Anderson Cancer Center
Houston, Texas
Presenting Author(s)
Co-Author(s)
Background:
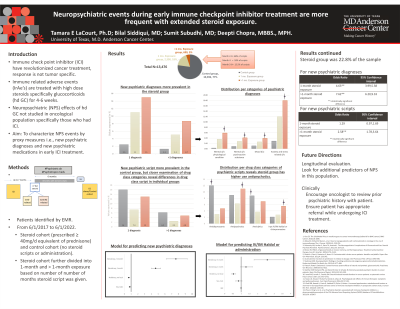
While immune checkpoint inhibitors (ICI) have revolutionized cancer treatment, they can also cause immune related adverse events (irAE’s), especially in the first months of ICI treatment. The majority of irAE’s are treated with high dose (hd) steroids for 4-6 weeks. HD steroids pose a risk factor for neuropsychiatric events in other populations; this has not been characterized in –potentially more vulnerable- cancer patients undergoing ICI treatment. Our objective was to describe the incidence of neuropsychiatric events after hd steroid prescription in patients undergoing ICI.
Methods:
For this retrospective longitudinal two-cohort study (steroid and control cohort), we used data from electronic health records (EHR) to identify patients who received ICI between [6/1/2017] and [6/1/2022]. Collected EHR data included hd steroid prescriptions within 7 months of ICI onset and, for neuropsychiatric events, the number and type of new psychiatric diagnoses (recorded ICD10-codes) and new inpatient psychotropic medication within 6 months after the 1st steroid prescription or an equivalent date for patients who did not receive hd steroids.
Results:
A total of 3080 patients received hd steroids within 7 months of ICI onset (“Steroid group”) and 10,396 patients did not (“Control group”). Demographic characteristics for Steroid vs. Control groups are: mean age 62 vs. 63; % female 41 vs 41; %non-white 19% vs. 20%. Within the Steroid group, 78% (2,390) had a single hd steroid exposure (i.e., one month with hd steroid prescription) and 23% (690) had repeated steroid exposure (i.e., >1 month with hd steroid prescriptions) in the 6 months from first steroid prescription. Compared to Controls, patients in the steroid group had a higher incidence of new psychiatric diagnoses [Steroid vs. Control: 17% (536) vs. 3.8% (399)] and of inpatient administrations of chlorpromazine/haloperidol [3.4%, 2.1%]. Within the Steroid group, those with repeated exposure had a higher incidence of new psychiatric diagnoses [Repeated vs. Single: 23% vs. 16%] and a higher incidence of inpatient administrations of chlorpromazine/haloperidol [5.5% vs. 2.8%]
Conclusion:
Psycho-oncologist may want to be alert for neuropsychiatric events in patients receiving hd steroids, especially when exposure to steroids is repetitive.
Presentation Eligibility: Not previously published.
Presented preliminary data at APOS 2024 meeting. However, current analyses is more comprehensive and complete.
Diversity, Equity, and Inclusion: Our topic is applicable to many oncology patients regardless of their ethnic background.

